Historically, Central Manchester has been an area with a high spend and yet relatively poor outcomes in type 2 diabetes; it also sits within Greater Manchester, which is among the areas with the worst cardiovascular outcomes in England (Public Health England, 2019; 2021). Furthermore, it has very much been an outlier as one of the few areas in the country that has had no community diabetes provision, despite widespread evidence of benefit from integrated diabetes services in the literature (Nicholson et al, 2016; Diabetes UK, 2017).
Numerous models of integrated diabetes care services have existed for some considerable time and have been well documented. But what would be the challenges and the enablers for a small diabetes team arriving “late to the party” to integrate diabetes care within Central Manchester? Could a model of type 2 diabetes care be implemented to promote timely and holistic primary care management, with integration of secondary, primary and wider community services? This model would deliver education to the multidisciplinary team of healthcare professionals (HCPs) and provide support and education to people with diabetes, their families and their carers throughout their diabetes journeys.
This article, through a series of key areas, sets out to discuss the experiences of two Community/Primary Care Diabetes Specialist Nurses who inherited a blank canvas in one of the few remaining areas of the UK naïve to a community diabetes service, and transformed it into a vibrant and varied palate of bespoke diabetes care, to fit with the brief previously outlined.
Background
CoDES (COmmunity Diabetes Education and Support) was established in April 2018 as a two-year pilot project commissioned by Manchester Health and Care Commissioning, under the clinical governance of Manchester University NHS Foundation Trust, designed to scope opportunities and look at best working practices related to introducing a long overdue integrated type 2 diabetes community service within Central Manchester.
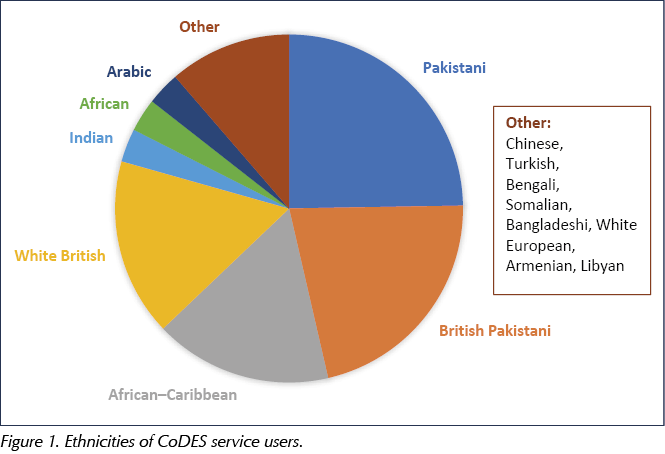
The CoDES pilot was formulated ahead of the formation of the Primary Care Networks in England and was thus allocated to what was then a neighbourhood of seven GP practices within an area with significant social deprivation (one of the lowest Indices of Deprivation in England), poor health literacy and a highly cosmopolitan demographic of residents from a wide variety of ethnic backgrounds (Figure 1). During the second year of the pilot, the CoDES team expanded to work with a total of 12 GP practices.
The ensuing sections set out the key approaches CoDES adopted in striving to attain the desired goals relating to diabetes education and support. These approaches included listening to service users, with subsequent bespoke delivery of services to meet specific needs. We embraced all formats of educational delivery in addressing identified knowledge gaps, both for HCPs and for people with diabetes, and looked beyond glycaemic control to encompass holistic diabetes care. Uniquely, there was integrated working with commissioners, creating solutions to local DSN workforce shortages and capturing data to ensure onward business planning for the continuation and expansion of CoDES as a sustainable model of care.
Listening to service users and delivering bespoke services meeting population needs
In its infancy, the priority for CoDES was to engage with all practices, with the clear realisation that a “One Model Fits All” approach was inappropriate. There was an early realisation that each practice had different levels of ability and capacity to deliver diabetes care but also, most importantly, that they were the ones that understood their demographics and populations, and thus knew what would work best for their service users. It was the role of CoDES to listen and match its service to their varied needs. Therefore, for example, in one practice with a small type 2 diabetes case load, there were monthly dedicated practice nurse mentoring clinics, whereas in a larger practice there were twice-weekly clinics, with a blend of direct delivery by the CoDES team, mentorship to all levels of HCPs and virtual clinics. In another practice, there were weekly face-to-face clinics delivered by CoDES, and support with group consultations.
As an ongoing process, CoDES has sought to listen to and understand the feedback of those in our care – both people with type 2 diabetes and their HCPs – and to act on their suggestions for improving care and education. We were pleased that, in a snapshot survey of people with diabetes and HCPs in July 2019, 32 of 32 (100%) responded to say that they would recommend the service to others and felt we had listened to their needs.
Embracing all educational delivery formats in striving to bridge the gap in educational needs for all HCPs working in diabetes care
With only two DSNs working within the CoDES team (1.9 whole time equivalents) and an estimated 2671 people registered with type 2 diabetes within the neighbourhood of practices (2018 data), it was never going to be a feasible model to have the CoDES team deliver all diabetes care to everyone. Thus, the biggest emphasis within the CoDES objectives has been on the delivery of education to HCPs, to include all multidisciplinary HCPs involved in diabetes care, as well as wider community and social care support groups, so that a ripple effect in terms of optimal care and management could evolve.
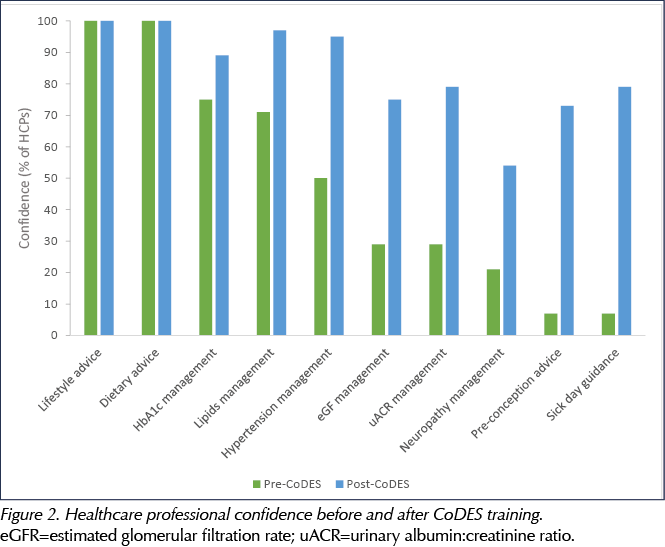
At 2 years, CoDES has delivered education to over 1750 HCPs, wider community workers and volunteers. This has been a blend of face-to-face mentorship and preceptorship; virtual support including monthly multidisciplinary team meetings between primary care and secondary care clinicians; advice and guidance by email or phone; and formal educational events. Particularly positive feedback has been given for the monthly dissemination of the CoDES Hot Topics in Diabetes newsletters, which are now circulated beyond the CoDES practices across all areas in Manchester, and the HCP Resources Pack, a directory of useful information and signposting links that is updated regularly to ensure its contemporaneous status. Lest we forget, those working in primary care have more than diabetes to focus on, and the very necessity to be a generalist makes it challenging to keep abreast of all changes in all areas, so it is of paramount importance that we serve to provide timely updates in easy-to-use formats. Feedback from educational activities has been highly positive, and an educational needs analysis undertaken at 1 year showed a significant improvement in the confidence levels of HCPs in managing some of the essentials of diabetes care, whilst illustrating the direction of areas for further educational input (Figure 2).
Looking beyond glycaemic control to deliver holistic care by managing diabetes and preventing cardiovascular and renal disease
With diabetes and cardiovascular disease (CVD) intrinsically linked, and in an area with some of the poorest CVD outcomes in the UK, a priority for the service has been to deliver holistic diabetes care focusing not just on glycaemic control but also on optimising blood pressure (BP) and lipid control, and supporting proactive cardiorenal protection where appropriate. Data from the Steno-2 study shows that doing relatively simple things well will have major positive benefits for those living with type 2 diabetes, including reduced long-term morbidity and mortality, fewer hospital admissions and economic benefits (Gaede et al, 2003; 2008; 2016). Cardiorenal outcomes are likely to be further enhanced with appropriate use of certain sodium–glucose cotransporter 2 inhibitor (SGLT2i) and glucagon-like peptide-1 receptor agonist (GLP-1 RA) therapies (Nagahisa and Saisho, 2019).
As shown in Figure 3, baseline data defined that the “average” person reviewed in a CoDES Primary Care Clinic was aged 57 years, with a diabetes duration of 11 years and an HbA1c of 81 mmol/mol (9.6%). Although BP and lipids were generally well controlled, one in four individuals had already had a CVD event and just under 40% already had chronic kidney disease, defined as an estimated glomerular filtration rate less than 60 mL/min/1.73 m2 and/or a urine albumin:creatinine ratio (uACR) above 3 mg/mmol, this being an important risk factor for future CVD events (Winocour, 2018).
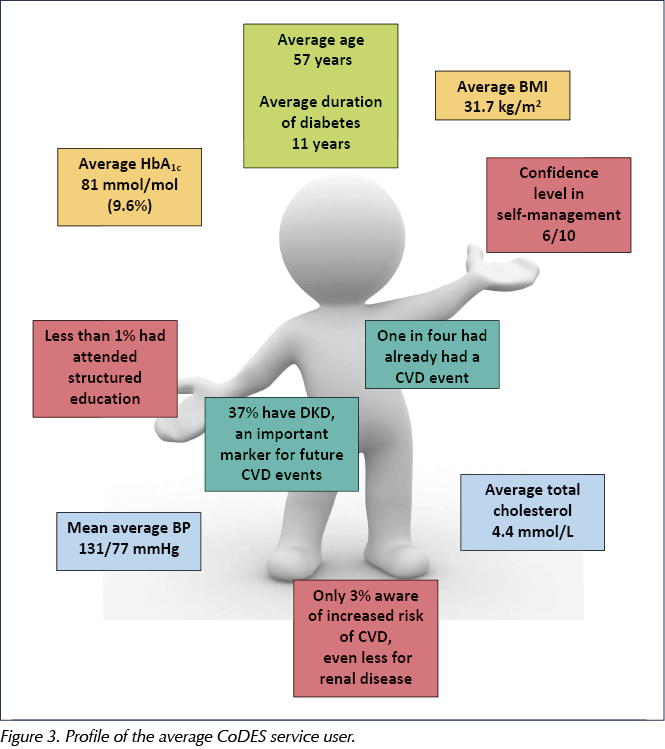
Significantly, one in four people seen were under the age of 50 years, with the vast majority presenting with suboptimal glycaemic control and many with diabetes complications already developed. These younger age groups are likely to be reflective of the higher proportion of people from ethnic minority backgrounds within the CoDES population, in whom type 2 diabetes onset is often from an earlier age. These relevant data also show that, although the average BMI was just under 32 kg/m2, the most common BMI range was 25–29 kg/m2, highlighting the need to consider screening for type 2 diabetes at a younger age and lower BMI within certain populations, so that we might better capture and manage the condition earlier and look to prevention and remission in a timelier manner (Wright et al, 2020).
Using a bespoke, evidence-based care pathway developed by local diabetologists and the CoDES service for the whole Greater Manchester area, there has been a positive implementation of appropriate cardioprotective diabetes education and medications in those with established CVD or high CVD risk. As the service progressed, a similar evidenced-based diabetes–renoprotection pathway was also put in place. These interventions to improve cardiorenal outcomes were relevant for the 26% of the people the CoDES service reviewed who had coexisting diabetes and atherosclerotic CVD or heart failure, and the 37% of those who had coexisting CKD.
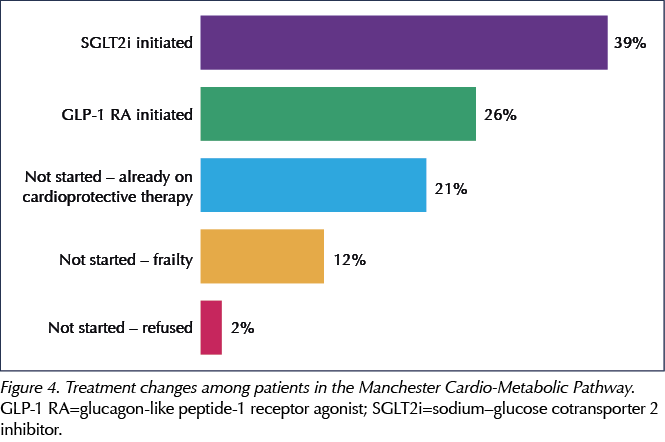
For the 26% of persons identified as suitable for management as per the “Manchester Cardio-Metabolic Pathway”, 20% had established atherosclerotic CVD and 6% had heart failure. Of this group, 21% were already on suitable therapies, 39% were started on an SGLT2i and 26% on a GLP-1 RA, while 12% were considered too frail and 2% refused (Figure 4). Research suggests that the prevalence of heart failure amongst those with type 2 diabetes is around 9.5–22.3%, depending on the population studied (Boonman-de Winter et al, 2012). Thus, CoDES data suggest an under-diagnosis of heart failure and a need to consider screening in those with risk factors for the condition.
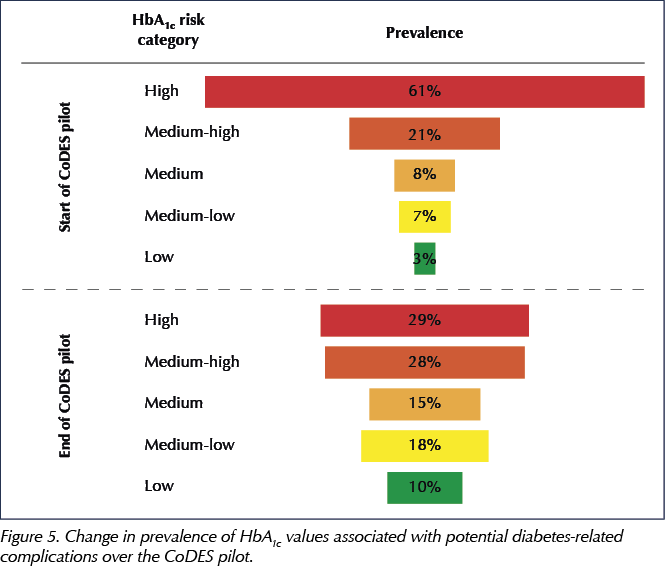
In those with suboptimal BP (systolic BP >140 mmHg) and lipids (total cholesterol >4.0 mmol/L) , 88% (BP) and 95% (lipids) showed improved levels, with 76% and 79% respectively achieving Quality and Outcomes Framework (QOF) targets of BP <140/80 mmHg and total cholesterol <5 mmol/L. Within the cohort directly reviewed by the CoDES team, the average HbA1c fell from 81 to 64 mmol/mol (9.6% to 8.0%), with the number of people with an HbA1c <75 mmol/mol increasing by 50%. Figure 5 illustrates the change in prevalence of elevated HbA1c values associated with potential diabetes-related complications to lower values associated with less risk over a period of 12 months.
In achieving improved HbA1c values, all individuals were given a refreshment of education, a motivational approach to encouraging lifestyle changes and signposting, where appropriate, to local and national support resources such as structured education. In addition, 48% of the CoDES population had an escalation of their oral hypoglycaemic medication. Overall, 29% of people were optimised onto injectable therapies at first review, with 16% starting on a GLP-1 RA and 13% commencing insulin. A further 29% who were already using insulin received support such as titration of doses, optimisation of injection technique or a change of regimen (Figure 6). A guideline on the safe use of insulin, including appropriate insulin titration, was produced for HCPs and is now hosted on the Greater Manchester Medicines Management Guidelines website (available at: https://bit.ly/3dFPk6L).
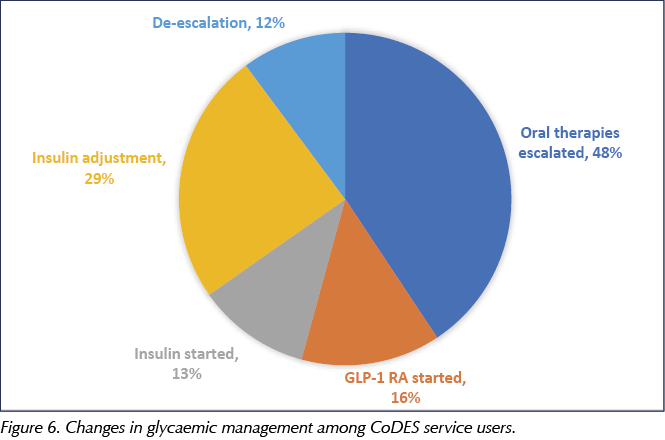
Medication adjustment in response to changes in patient characteristics was required in 11% of individuals to ensure on-label use as per the Summaries of Product Characteristics, while 12% of people required their medications to be de-escalated, for reasons including hypoglycaemia in those prescribed insulin and/or sulfonylureas, and in other medications where there had been a lack of efficacy.
Addressing gaps in education for those living with type 2 diabetes
Addressing the shortfall in awareness of the implications of type 2 diabetes and effective education are vital for improving diabetes-related outcomes; however, CoDES data showed that less than 1% of people attending for review in a CoDES Clinic had attended structured diabetes education (Figure 3). Less than 3% of people seen understood that diabetes could contribute to cardiovascular and/or renal complications. This lack of awareness can heighten non-attendance and create difficulties for people in understanding the reasons for lifestyle changes and in taking medications (Chatterjee et al, 2018).
Education for those under the care of CoDES has been challenging in an area where English is often not the first language and the average literacy age is low. There was an early realisation of a need to adapt resources to develop pictorial questionnaires, posters for waiting areas and a range of culturally appropriate resources for those in our care. CoDES is also continuing to work with the Greater Manchester Strategic Clinical Network on improving access to structured education, to include enrolling people in the My Diabetes My Way digital app, which is a testbed bid currently being evaluated by Manchester University. CoDES has also supported practices with group consultations, enabling education and peer support to those with type 2 diabetes and their families and carers. Within the service, there is a strong emphasis on links to social prescribing initiatives and wider community support, including local IAPT services.
Integrated working with commissioners
A member of the CoDES team has uniquely worked within the local commissioning organisation, Manchester Health Care and Commissioning (MHCC), for a fixed period (two days a week for 9 months), recognising that this placement would allow the articulation of the voices of people with type 2 diabetes and those HCPs at the coal face of care to key decision-makers in service delivery. One example of this strategy working well was in relation to diabetes pre-conception care. MHCC has developed the Manchester Primary Care Standards, which, through a novel approach, financially incentivise practices to deliver care beyond QOF requirements (Meadowcroft, 2020). The delivery of pre-conception advice to all women with diabetes of childbearing age has been one such Standard, and CoDES, along with other local stakeholders, was highly influential in developing the Standard and delivering the educational support required across the city. All practices were required to provide evidence that at least one practice nurse and one GP had completed a national online training module relating to diabetes and pre-conception care co-authored by a CoDES Team member (PCDS, 2019; available for free at: https://bit.ly/32FMUyN), and to code that pre-conception advice had been given where relevant. At 1 year, data showed that 65% of all eligible women had been recorded as having received appropriate pre-conception advice, compared with a baseline in which there was no record of receiving this advice. HCP confidence in delivering pre-conception advice has increased from 7% to 73% with the support of the CoDES team (Figure 2).
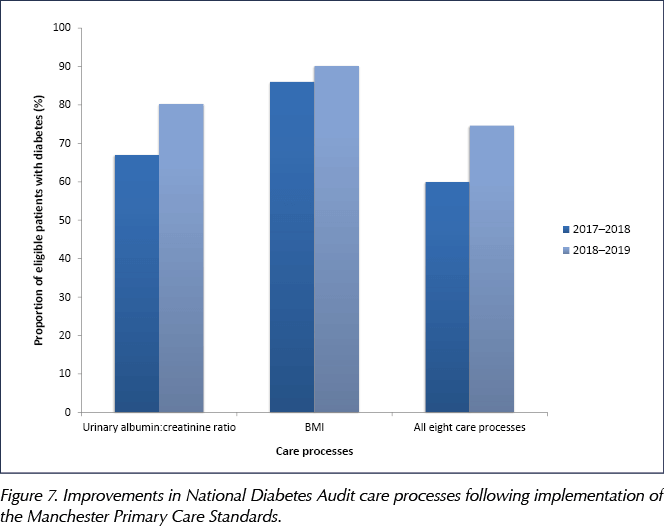
A further Manchester Standard incentivised GP practices to record BMI values and uACR results, which no longer sit within QOF indicators but which are recognised as being of high value when reviewing a person with diabetes. Indeed, a positive uACR result is often the first signal of renal decline, and yet nationally this is the care process that has the lowest level of achievement (NHS Digital, 2020). At 1 year, an audit of performance against the Standards showed that the proportion of people achieving all care processes across MHCC had increased from 59.9% to 74.7%, while the proportion receiving uACR tests had increased from 67.0% to 80.3% (Figure 7). Although measuring uACR does not always translate into intervention if the result is positive, it is encouraging that, thanks to CoDES educational activities, HCP confidence in the management of a positive uACR result has increased from 29% to 79%.
Addressing DSN workforce shortages
Creating solutions to workforce shortages has been an important consideration for CoDES as, mirroring the national picture (Hicks and James, 2020), there is a shortfall of experienced DSNs to recruit within the locality. CoDES has been innovative in recruiting a practice nurse with an interest in diabetes to provide service leadership, which has allowed the service to develop in a “bottom-up” approach sensitive to the demands and scope of primary and community care. This approach has been referenced in positive service feedback from HCPs. The other CoDES team member is a highly experienced secondary care nurse, which has been significantly beneficial in terms of forging relationships and links with community and inpatient care. This team member was new to diabetes as a speciality and to working in primary care; however, successful diabetes training and education, professional development and clinical governance were enabled in tandem with the secondary care diabetes team. Our experience provides evidence of an ability to successfully recruit and train diabetes-naïve nurses, which is paramount to CoDES’ ongoing sustainability and development.
Allowing sufficient time for data capture and business planning
Throughout the service’s inception, design and roll-out as a pilot, the challenge of being re-commissioned was never far from our thoughts. Woven through all CoDES interactions and clinics has been the need to capture data to show activity and performance. At times this has been burdensome due to time constraints; however, importantly, it has allowed thorough analysis of outcomes. The data have served as a powerful tool in terms of providing high-quality information for a timely investment review and business planning proposal, in which CoDES was successful in securing ongoing funding and team expansion. The review process for this future funding began 10 months prior to the date of pilot completion. Given that the service was only fully functioning three months after inception, this gave just an 11-month time period to show activity and outcomes, illustrating the challenge of needing to show outcomes at speed from the start of a new service.
Financially, based on prevented referrals to secondary care, the CoDES pilot demonstrated estimated savings of £282 000 (£120 000 in 2018/19 and an estimated £162 000 in 2019/20). The cost of the service was £246 000, resulting in an overall return on investment. However, it is useful to note that this was not a comprehensive economic analysis because it does not take account of changes to medication or the impact on hard outcomes such as diabetes-related complications and hospital admissions.
Although it is widely acknowledged that a purely glucose-centric approach to diabetes management is not appropriate in reducing the macrovascular burden of type 2 diabetes, CoDES did model HbA1c outcomes data using an IMPACT Tool (Baxter et al, 2016), which showed the potential for a reduction in spend on microvascular complications (retinopathy, neuropathy and nephropathy damage) over 5–25 years. The cost of doing nothing (i.e. having no intervention from the CoDES team), based on these three complications across central Manchester, was estimated to be £12 746 064 over 25 years.
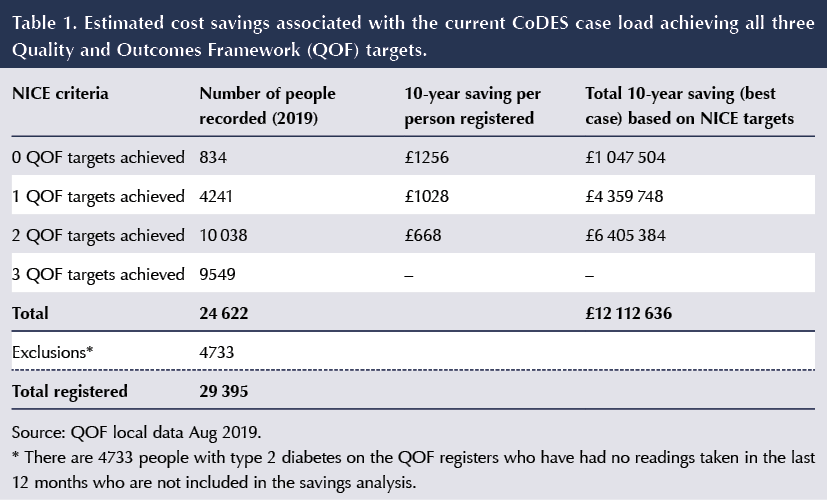
We also looked at financial modelling based on economic research predictions by the Nuffield School of Economics (Keng et al, 2019), which showed the potential savings over 10 years for achieving one, two or all three of the national QOF treatment targets of HbA1c, BP and lipids per person with type 2 diabetes. Among the population of 29 395 people with type 2 diabetes across the footprint of the MHCC (which includes North, South and Central Manchester), the application of CoDES education and support to enable achievement of all three QOF targets could result in a saving of over £12 million over 10 years (Table 1).
COVID-19 and future developments
The COVID-19 pandemic, as in many other healthcare areas, has taken its toll on the CoDES model of service design and the monies for planned expansion. The start of the pandemic coincided with the end of the CoDES pilot and, naturally, HCPs became too busy, either at the COVID-19 frontline or supporting it, to be focused on diabetes educational needs. By necessity, the CoDES service became more of a hands-on model of care, delivering advice and guidance and directly reviewing people with diabetes, with over 5500 direct contacts from March 2020 to March 2021, a period of time in which the team had one member re-deployed to critical care for 3 months. The number of these direct contacts is spiralling upwards as we face increasing demand for support against the backdrop of the resetting of routine diabetes services without any increase in capacity. This is a powerful reminder that a community diabetes service that provides personnel to deliver diabetes care has a greater challenge to be sustainable than one which teaches and supports other HCPs within larger teams to deliver diabetes care. With this in mind, we are currently in the process of refocusing the service to the original model, with the emphasis on education rather than active clinics.
The recently published guideline Best Practice in the Delivery of Diabetes Care in the Primary Care Network (Ali et al, 2021) will allow for Primary Care Networks (PCNs) to strengthen their diabetes care and create sustainability at whatever stage of development they may be in, and CoDES looks forward to serving at the tier 3 level in support of PCNs, and continuing to listen, to innovate, to evolve and to offer educational support.
Conclusion
The CoDES pilot, with great local support and buy-in from HCPs and commissioners across primary, community and secondary care, has been successful in meeting its objectives. It has promoted holistic primary care diabetes management, with integration of secondary, primary and wider community care services. It has delivered on education to the multidisciplinary team of HCPs and has supported people with diabetes, their families and carers throughout their diabetes journeys.





Helping homeless adults to overcome the challenges of managing their condition.
16 Apr 2024