Study aim
The main aim of this study was to evaluate HRQoL, and the factors that may affect it, in children with type 1 diabetes, in comparison with their peers without the condition. The primary focus was on assessing the influence of type 1 diabetes upon children’s and their parents’ life. The secondary aims were to describe the role of parents in their children’s HRQoL and to highlight differences in measures of interest between children treated with multiple daily insulin injections and those on insulin pump therapy.
Methods
Sample
The sample consisted of 87 children aged 5–18 years who were diagnosed with type 1 diabetes and were attending the diabetes centre of the General Children’s Hospital P&A Kyriakou (a public hospital of the National Health System of Greece) and the diabetes outpatient setting of the Paediatric Hospital Mitera (a private hospital run by the health corporation Hygeia), and a comparison group of 119 peers without diabetes. One parent of each of the children with diabetes (n=87) and 29 parents of the control group also participated in the study.
The participants with diabetes were a convenience sample, while the control group was selected by lottery from the paediatric outpatient settings of the two hospitals. All had attended for minor health problems (e.g. diarrhoea, vomiting, cough, increased body temperature ≤38.0°C). Children with chronic conditions other than type 1 diabetes were excluded from the control group.
The study took place between June 2017 and September 2018. Approval was given by the Ethical Committee of each paediatric hospital. Informed consent was obtained by the parents of the participants, after making known the aims and process of the study, before handing in the assessments.
Inclusion criteria for entering the study were as follows:
- Young people aged 5–18 years with a diagnosis of type 1 diabetes according to International Society for Pediatric and Adolescent Diabetes criteria.
- Diagnosis of type 1 diabetes for at least 1 year before the study started.
- Willingness to participate in the study.
- Good knowledge of the Greek language in both children and parents.
- Absence of any psychiatric condition, mental handicap or genetic syndrome.
Instruments
The PedsQL 3.0 Type 1 Diabetes Module and the PedsQL 4.0 Pediatric Quality of Life Inventory (Varni et al, 2001; 2003) were used to assess HRQoL. Demographic data, including educational level of the parents, were evaluated using a separate demographics form.
The PedsQL 3.0 Type 1 Diabetes Module was designed to measure diabetes-specific HRQoL in people with diabetes. It consists of 28 items, grouped into five scales: diabetes symptoms (11 items); treatment barriers (4 items); treatment adherence (7 items); worry (3 items); and communication (3 items). A five-point response scale is used, ranging from 0 (never a problem) to 4 (almost always a problem). The items are reverse-scored and linearly transformed to a 0–100 scale (0=100, 1=75, 2=50, 3=25 and 4=0), and are then averaged to give an overall score of 0–100, with higher scores indicating better HRQoL. The instrument can be used by children and adolescents aged 5–12 years and their parent-proxies.
The PedsQL 4.0 Pediatric Quality of Life Inventory was used for the assessment of HRQoL in the control group. It is a 23-item tool encompassing four subscales: physical functioning (8 items); emotional functioning (5 items); social functioning (5 items); and school functioning (5 items). The format, instructions, Likert-type response scale and scoring method are identical to the Type 1 Diabetes Module, with higher scores indicating better HRQoL. The emotional, social and school functioning subscales (15 items in total) can be averaged to obtain a psychosocial health summary score.
A three-step process of translating the questionnaire into Greek took place. First, two independent translators translated the original English versions into Greek. The two translators and the supervisor of the research compared the two Greek versions in order to obtain a final one. Next, each Greek version of the questionnaire was given to another two translators, who worked separately to each other, to perform a backward translation. Two back-translations were gathered. The two translators and the supervisor compared the back-translations of the questionnaire to obtain a final back-translated version. Finally, a panel of experts, consisting of two university professors, one paediatrician and two psychologists specialising in children, compared the original English version with the back-translation of the questionnaire. Minor changes regarding linguistic differences between the two texts and cultural adaptations were made. All the changes were made in the Greek version of the questionnaire. Before the questionnaire was translated into Greek, permission was obtained from the original author. A pilot study was conducted to test the PedsQL 3.0 Type 1 Diabetes Module before its administration to the children with diabetes and their parents.
Statistical analysis
Data analysis was conducted using SPSS Statistics 23.0 (IBM, Armonk, NY, USA). Continuous data were expressed as means ± standard deviation, while categorical and dichotomous variables were expressed as absolute values (n) and percentages of the groups. The Kolmogorov–Smirnov and Shapiro–Wilk tests were used to check the normal distribution of the continuous variables. The Student’s t-test and analysis of variance were used to determine whether quantitative variables that followed the normal distribution presented differences between groups. The Mann–Whitney U test was used when variables were not normally distributed. To assess the correlation between two variables, the intraclass correlation coefficient (ICC), Pearson’s r and Spearman’s rho tests were used; Pearson’s r was used for assessing the correlation between two quantitative variables that were distributed normally, while Spearman’s rho was used for variables that were not normally distributed. A two-tailed P-value less than 0.05 was considered to demonstrate statistical significance.
Results
The demographic characteristics of the young people who participated in the study are shown in Table 1. The mean age of the participants with type 1 diabetes was 12.64 ± 3.8 years, while the mean age of the comparison group was 12.17 ± 3.89 years. Overall, 46.0% (40/87) of the children with type 1 diabetes were using an insulin pump. The mean HbA1c was 57.6 ± 10.8 mmol/mol (7.42 ± 0.99%).
HRQoL of participants with diabetes (self-reports)
The mean overall HRQoL score was 81.87 ± 9.51 among children (aged 5–12 years) and 77.76 ± 11.19 among adolescents (aged 13–18 years). The difference in overall scores between the age groups was not significant (t=1.85; P=0.07); however, a significant difference was found in the “treatment adherence” (90.71 ± 10.42 vs 85.29 ± 12.48; z=–2.16; P=0.03) and “worry” (86.67 ± 15.01 vs 70.44 ± 18.70; z=–4.08; P<0.001) subscales, whereby children reported better HRQoL compared with adolescents (Table 2). Insulin pump users reported better HRQoL than their peers who used multiple daily injections on the “treatment barriers” (83.28 ± 13.97 vs 73.27 ± 17.18; z=–2.93; P=0.004) and “treatment adherence” (90.45 ± 11.65 vs 86.09 ± 11.52; z=–2.10; P=0.035) subscales. No significant difference was found between insulin pump and multiple daily injection users in terms of overall scores (82.22 ± 10.76 vs 77.90 ± 9.95; t=–1.95; P=0.055).
Participants were asked to rate their overall health status as “poor”, “average”, “good” or “perfect”. There was a link between mean HRQoL scores and self-reported health status, with higher HRQoL scores observed in participants who rated their health as perfect compared with those who rated it as good (82.67 ± 8.71 vs 75.03 ± 11.99; t=5.62; P=0.005). Those who were participating in any kind of sporting activity reported better HRQoL than those who did no sport (81.06 ± 9.97 vs 75.05 ± 11.54; t=–2.16; P=0.034). There was a significant negative correlation between HRQoL and age, with younger patients reporting better HRQoL than older ones (r=–0.26; P=0.015). Significant negative correlations were also found between HRQoL and weight (rho=–0.27; P=0.013), height (rho=–0.22; P=0.044) and number of insulin injections per day (rho=–0.26; P=0.02). No other factor was found to correlate significantly with HRQoL.
HRQoL of participants with diabetes (parental reports)
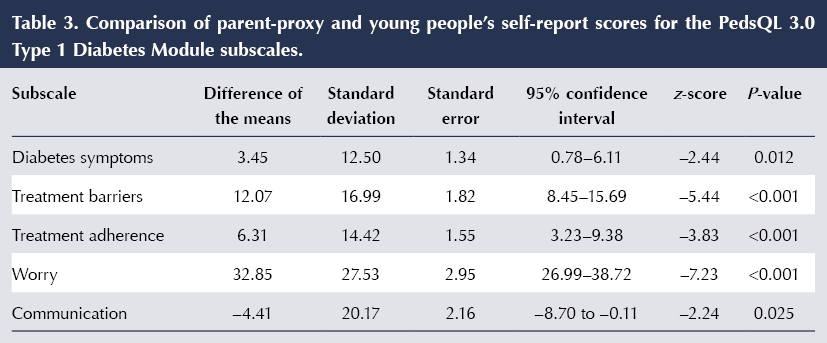
There was a significant correlation, of moderate intensity, between young patients’ self-reports and parental scores (r=0.61; P<0.001, and ICC=0.599; P<0.001). However, parents tended to underestimate their children’s HRQoL (t=7.01; P<0.001). Table 3 summarises the comparison of HRQoL scores from the participants’ and parents’ reports. The young people reported higher mean HRQoL scores than their parents for all the subscales of the tool, with the exception of the “communication” subscale, for which parents gave higher scores than their children (t=–2.24; P=0.025).
Parents whose children rated their own health status as better perceived significantly higher HRQoL in their children than those whose children rated their health status as worse (F=3.37; P=0.04). Moreover, there was a small but significant negative correlation between parental reports of HRQoL and hypoglycaemia (rho=–0.25; P=0.02).
HRQoL of young people with versus without diabetes (self-reports)
While mean HRQoL scores were lower in children with diabetes than in those without (Table 4), the difference between the groups was not significant.
HRQoL of children without diabetes (parents’ reports)
The mean HRQoL score was 78.27 ± 13.78 for the children without diabetes and 85.12 ± 10.40 for their parents. A significant difference was found between these scores, irrespective of age category (z=–2.62; P=0.008).
Discussion
Our results show a high mean HRQoL score in young people with type 1 diabetes, which was not significantly different to that of their peers without the condition. This finding is in accordance with the results of Laffel et al (2003), who found that children and teenagers without diabetes reported the same HRQoL as paediatric patients with the condition. Moreover, in both studies, parent-proxy reports tended to underestimate the children’s HRQoL in comparison with parents of children without diabetes, who tended to overestimate their children’s HRQoL.
Many studies have observed high mean HRQoL scores among young people with type 1 diabetes (Laffel et al, 2003; Nathan et al, 2005; Abolfotouh et al, 2011). Stahl et al (2012) reported that children with type 1 diabetes were more likely to rate their health as “excellent” in comparison to peers without the condition. They also found no difference between the young patients’ self-reported HRQoL scores and those of their peers. In accordance with Stahl and colleagues, we observed a significant difference in HRQoL scores between those participants who rated their health status as “perfect” and those who rated it as “good”. Similar findings were observed by Abolfotouh et al (2011), who found that over 80% of participants reported a high level of HRQoL and 38% rated their health status as “good”.
Almost half of the participants in our study were using an insulin pump to control blood glucose. The results showed a slight increase in mean HRQoL scores with insulin pumps compared with insulin injections, although there was no significant difference in overall scores. Furthermore, the number of insulin injections per day significantly affected participants’ HRQoL, with fewer injections per day associated with better HRQoL. Valenzuela et al (2006) observed no impact of insulin pump use upon young people’s HRQoL. Insulin pumps, as part of an intensive treatment regimen, can play a vital role in the management of the condition, resulting in a better HRQoL for both young people and their families. Many studies have shown the superiority of insulin pumps in achieving glycaemic control and decreasing hypoglycaemia compared with multiple daily injections (Jakisch et al, 2008). One explanation for this is that young people can use the pump to administer small doses of insulin, which can help to prevent serious hypoglycaemia in those with low daily insulin requirements (Phillip et al, 2007; Jakisch et al, 2008).
The existing literature suggests that demographic factors, such as the individual’s age, birth weight, age at diabetes diagnosis, body weight and stature, as well as HbA1c, play an important role in the impact of diabetes on HRQoL (Little, 2003; Wagner et al, 2005; Tahirovic et al, 2012). In our study, age, weight, height and the number of insulin injections per day were found to have a significant negative correlation with HRQoL. Our study cohort had a mean HbA1c of 58 mmol/mol (7.5%), implying good blood glucose control and management of type 1 diabetes. Tahirovic et al (2012) found that young people whose HbA1c levels were under 64 mmol/mol (8.0%) reported better HRQoL and metabolic control than those with higher HbA1c. Wagner et al (2005) also found that HbA1c levels under 64 mmol/mol were correlated with better HRQoL, and Kalyva et al (2011) showed that various demographic factors, including low HbA1c, were correlated with HRQoL.
Our study suggests that parental occupation (both mothers’ and fathers’ jobs) was not significantly associated with young people’s HRQoL. Similarly, Al-Akour et al (2010) found that mothers’ and fathers’ employment status was not significantly associated with HRQoL. However, other studies have found that socioeconomic level was associated with HRQoL (Huang et al, 2004; Hassan et al, 2006). In our study, this lack of association was observed in both the young participants’ self-reports and parent-proxy reports, as well as in the control group and their parents’ reports.
In our study, the majority of the young people with and without diabetes participated in sporting activities, and those who did so reported better HRQoL. Other studies support this finding, showing that sporting activities can help to maintain good glycaemic control and decrease HbA1c levels (Beraki et al, 2014; Martínez-Ramonde et al, 2014).
Study limitations
This study has a number of sources of potential bias that may limit the generalisability of the results. The HRQoL assessments were performed using questionnaires and scales, a method that may often result in a number of biases, as outlined by Choi and Pak (2005). In addition, the sample consisted of participants from two paediatric hospitals, one of which was a private hospital, and this may have led to selection bias caused by systematic differences (e.g. gender, socioeconomical status, etc.) between the participants of the sample and the general population. Furthermore, the size of the sample was small and this should be taken into consideration. A further limitation was the study’s cross-sectional design; longitudinal studies evaluating the effects of demographic factors and other interesting variables on HRQoL of young people with type 1 diabetes and their families are necessary.
Conclusions
In our study, young people with type 1 diabetes reported good HRQoL, by improving metabolic control (HbA1c <64 mmol/mol), adhering to intense insulin therapy regimens and participating in sporting activities. Although a negative correlation was found between higher daily numbers of insulin injections and HRQoL, it seems that young people with diabetes can cope with this in order to achieve better metabolic control, which itself improves HRQoL. Reductions in the number of insulin injections per day and in hypoglycaemia can improve the HRQoL of young people and their families. It also seems that the use of insulin pumps has increased among young people in Greece between June 2017 and September 2018. Even though our results did not show a significant superiority of insulin pumps compared with injections, we believe this would be demonstrated with a larger sample size.
The parental reports tended to underestimate young patients’ HRQoL, with parents believing that the condition negatively affects every aspect of their children’s daily life. Despite their condition, the majority of the young people rated their health status as “good” or “perfect”. Parents can play a vital role in the effective management of their children’s type 1 diabetes by participating actively in treatment and supporting them with the demands of the condition.








Helping homeless adults to overcome the challenges of managing their condition.
16 Apr 2024