In May this year, a consensus report, funded by the American Diabetes Association (ADA), on the role of medical nutrition therapy (MNT) in the management of diabetes and non-diabetic hyperglycaemia was published (Evert et al, 2019). It highlights the importance of the dietary treatment of diabetes at all stages of management and prevention. The headline is a simple one:
HbA1c reductions from MNT can be similar or greater than what would be expected with medication for type 2 diabetes.
Report summary
- MNT is a cost-effective treatment for diabetes. Improvements in glycaemic control can be similar or greater from MNT than improvements brought about by medications. Advice from a dietitian with specialist knowledge in diabetes is a priority to enable people with diabetes to identify their own areas for change. There is no “one-size-fits-all” diet for diabetes, and patients can be guided towards healthy, sustainable eating and exercise patterns to achieve realistic targets using a variety of approaches to suit them.
- Weight reduction is a highly effective treatment for type 2 diabetes prevention and management at any stage of the condition. Success increases with greater patient engagement with a programme and making lasting lifestyle changes.
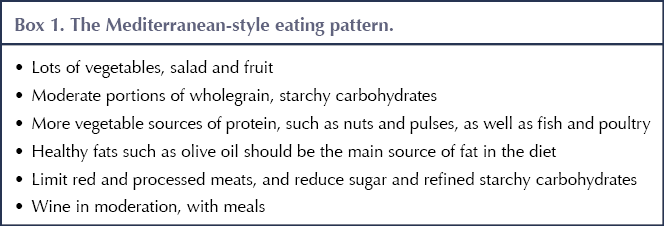
- The Mediterranean-style eating pattern should be recommended as the new “healthy eating” for glycaemic control and cardiovascular disease (CVD) risk reduction.
- Reducing overall carbohydrate intake can improve glycaemia. Most recommended dietary patterns will lead to a reduction in carbohydrate intake, and low- and very-low-carbohydrate diets can be useful in certain circumstances.
- Common themes in all diets that have been found to be successful are:
– More non-starchy vegetables.
– Minimise added sugars and refined grains.
– Choose whole foods over highly processed foods.
– Advise on appropriate portion sizes to achieve calorie targets. - Eating should continue to be a pleasure, and framing changes as positive and enjoyable will help maintain long-term change.
In more detail
The report is a consensus statement collated from recent evidence and expert opinion, and confirms what many of us have seen in our practice: people with diabetes can make a huge difference to their condition through dietary change and managing weight effectively. Dietary change should be the cornerstone of the treatment of diabetes.
The report has many similarities and some differences to the Evidence-based nutrition guidelines for the prevention and management of diabetes published by Diabetes UK (DUK) in 2018 (Dyson et al, 2018), some of which will be discussed below.
Individualised advice
The report stresses the importance of individualised nutrition advice or, as described here, MNT. The authors specifically recommend three to six encounters with a registered dietitian in the first 6 months after diagnosis and an annual review after that. MNT is described as a cost-effective component of the treatment of diabetes which has been shown to have a similar or greater effect on HbA1c as currently available medication.
The DUK guideline recommends that a dietitian with expertise in diabetes guide the nutrition advice of those with diabetes or non-diabetic hyperglycaemia. It states that there is good evidence for the benefit of structured diabetes education programmes which include advice on nutrition and self-management support.
Both reports agree that expert dietary advice for all people with diabetes should be an integral part of treatment. Consequently, the availability of specialist dietitians or health professionals with adequate time and skills to provide ongoing diet and lifestyle interventions should be a priority.
Type 2 diabetes prevention
For the first time, the ADA’s consensus report includes advice for non-diabetic hyperglycaemia, or prediabetes. The provision of an intensive lifestyle programme for the prevention of type 2 diabetes is recommended, supported by ongoing dietary advice. Weight reduction of 7% or more on a diet that can be maintained by the individual is the most effective treatment. Evidence for the most effective dietary pattern is mixed, although benefit has been found from a Mediterranean-style eating pattern. There is evidence of the benefit of digital health tools as an addition to this to improve the accessibility of the programmes.
Weight and the prevention and management of type 2 diabetes
The best evidence for the benefit of nutrition intervention is from weight reduction, with a loss of 5% improving glycaemic control and greater benefit seen with greater weight loss, and potential remission of type 2 diabetes seen with weight loss of 15 kg.
The consensus report supports the DUK guidelines in stating that there is no evidence that any one specific dietary pattern is more effective than others in promoting weight loss; advice needs to be individualised to suit the needs and lifestyle of the patient.
The possibility of remission of type 2 diabetes is discussed. This is related to weight reduction, and the DiRECT trial shows that remission rates increase with greater weight loss (Lean et al, 2018). When patients achieved a 15 kg weight reduction, there was an 86% remission rate at 1 year with no diabetes medication. There is a suggestion from a study by Esposito et al (2014) that food quality also matters – a reduced-carbohydrate, Mediterranean-style eating pattern was found to be more likely to induce remission than following a low-fat dietary pattern despite there being little difference in weight reduction.
The report also promotes advice on weight reduction alongside other treatments for weight loss. MNT will increase the effect of hypoglycaemic medications that promote weight reduction, weight loss medications and bariatric surgery.
Carbohydrate
In accordance with the DUK guideline, the consensus report also states that there is no optimal percentage of calories from carbohydrate, protein and fat, so people with or at risk of diabetes should adapt their diet based on individual preferences and requirements. The report also goes on to say, more strongly than the DUK guideline, that reducing overall carbohydrate intake has demonstrated the most evidence for reducing glycaemia. Many of the suggested eating patterns will necessarily lead to a reduction in carbohydrate intake as they involve reduction of sweet drinks and foods, and a reduced intake of refined starchy carbohydrate.
The report supports the use of a low- or very-low-carbohydrate diet as a viable approach in some people with diabetes, notably those not meeting glycaemic targets or for whom reducing antidiabetes medication is a priority. It is suggested, as would be the case in the UK, that specialist advice should be provided for those on hypoglycaemic medications. Further evidence is needed before any recommendations can be made regarding low-carbohydrate intakes in those with chronic kidney disease, disordered eating patterns and in pregnancy.
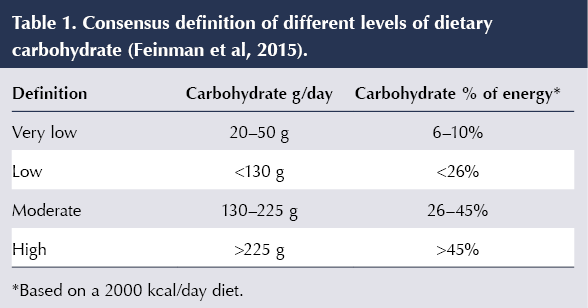
It should be noted that the definition of a low- and very-low-carbohydrate diet has varied between clinical trials, which makes direct comparison difficult. The values in Table 1 were developed by Feinman et al (2015), and have been used in UK reports.
Evidence of long-term benefit from a very-low-carbohydrate diet is not convincing because adherence can be a problem. This should be considered when advising on such diets, and individual advice should be given if a change in dietary pattern is required. Regular monitoring of glycaemic control should continue and medication should be adjusted as necessary.
Fibre
The consensus supports a high-fibre intake from dietary sources including whole grains and other natural plant sources. This is associated with lower all-cause mortality in people with diabetes (Burger et al, 2012). The consensus group suggests 14 g of fibre per 1000 kcal, which is in line with the UK recommendation of 30 g per day.
Fat
The report recommends replacing saturated fat with unsaturated fats to reduce total and LDL-cholesterol, and specifically replacing with monounsaturated fats from plant sources such as olive oil and nuts to reduce CVD risk.
Eating patterns
In both the ADA and DUK statements, the Mediterranean diet appears to have the strongest evidence in terms of its benefit in type 2 diabetes prevention, weight reduction, glycaemic control and reducing CVD risk. It is therefore logical that we could recommend the Mediterranean style of eating (Box 1) as the new “healthy eating”.
Other eating patterns with reasonable levels of evidence for benefit in terms of HbA1c and weight reduction include vegetarian and vegan, low- and very-low-carbohydrate, the DASH (Dietary Approaches to Stop Hypertension) diet and, at a lower level of evidence because of the different methods, intermittent fasting. Advice on these should be given on an individual basis, and different ways of eating will suit some more than others. A useful table illustrating the different dietary patterns used in the treatment of diabetes, and the supporting evidence, is given in the full report.
Pleasure of eating
The report states that maintaining, or increasing, the pleasure of eating should be considered a goal in any MNT, and positive messages should be given about “healthful” food choices. This is something that is not discussed in the DUK guidelines but should be an important consideration if we want people with diabetes to feel positive and empowered about the choices they are making, and confident that they can improve their health by changing eating habits.
Conclusion
The consensus report by Everts et al (2019) strongly supports the role of diet in the prevention and management of diabetes. When applying this to the UK, we need to consider how we can raise this issue as a priority in our management of patients, and how expert dietary advice by or guided by a dietitian with expertise in diabetes can be delivered. The main dietary messages are that weight management has the greatest effect on prevention of diabetes and glycaemic control; the Mediterranean eating pattern is recommended as the new healthy diet; and reducing carbohydrate intake can improve glycaemia – with the appropriate level of restriction to be decided on an individual basis. The pleasure of eating should also not be forgotten in our consultations with patients.
Resources
 |
Diabetes UK provides information about a range of diets for the management of type 2 diabetes, available here. These include meal plans for Mediterranean and low-carbohydrate diets. |
 |
Tools may vary in some aspects, but aiming to improve the overall style of eating is the goal.
The Mediterranean Diet Score Tool has been adapted from the PREDIMED trial. |
 |
Reference book for food values: Carb and Calorie Counter by Chris Cheyette and Yello Balolia. This and other reference books, as well as a carb and calorie counter app, are available at www.carbsandcals.com. |






Helping homeless adults to overcome the challenges of managing their condition.
16 Apr 2024