Diabetes decreases quality of life and disrupts people’s routine activities due to sickness, disability, early retirement or premature death, and loss of productivity (Breton et al, 2013). However, effective management improves the quality of life and productivity of people with chronic conditions (Hisashige et al, 2012). Type 2 diabetes management requires commitment to health-promoting behaviours, and behavioural changes are crucial in people with this condition; therefore, special attention must be paid to factors that can help empower these individuals (Greene et al, 2016).
Self-efficacy is one of the most important factors in behaviour change to support the proper management of diabetes (Graffigna et al, 2014). Self-efficacy is defined as the level of self-confidence required to efficiently perform a distinct behaviour within their ability (Hailu et al, 2019). Self-efficacy predicts adherence to blood glucose monitoring, diet, insulin injections and exercise (Miller and Rollnick, 2012). Tharek et al (2018) reported a significant correlation between higher self-efficacy and improved self-care in people with diabetes and concluded that self-efficacy plays a pivotal role in successful diabetes management.
Motivational interviewing (MI) is a counselling approach used by healthcare providers to help improve concordance with treatment recommendations (Szczekala et al, 2018). The primary purpose of MI is to reduce individuals’ perception of their disability in order to eliminate barriers and change successfully (Majd Abadi et al, 2018). MI increases the internal motivation of individuals and helps them explore and resolve ambivalence (Miller and Rollnick, 2012). In addition to increasing motivation, MI attracts the person’s attention to a specific topic, thereby allowing substantial changes in various behavioural patterns (Minkin et al, 2014). MI can be implemented individually and in groups due to its flexibility and ability to apply in different behavioural aspects (Lavoie et al, 2014). MI has been shown to be superior to traditional intervention strategies in addressing a wide range of psychological and physical disorders, including type 2 diabetes (Huffman et al, 2021).
Despite the rapid growth in the application of MI in different areas of healthcare worldwide, it is a novel approach, and limited research has been conducted into its effectiveness in Iran. Thus, the present study was conducted to investigate the effect of MI on self-efficacy in people with type 2 diabetes. Our hypothesis was that MI would improve self-efficacy in these individuals.
Methods
Study design and participants
This quasi-experimental study with a pre-test/post-test design was conducted in 2017. Participants were selected from people with type 2 diabetes who were members of the Bukan Diabetes Association in a city located in the northwest of Iran. In total, 60 participants were selected using a random numbers table. The participants were allocated into the control (n=30) and intervention (n=30) groups by drawing “A” and “B” cards. The sample size was determined based on the study by Navidian et al (2010), with a 95% confidence interval and 80% test power, using the GPower 3.1 software (Heinrich Heine Universität, Düsseldorf, Germany).
The inclusion criteria were as follows: (1) willing to participate in the study; (2) having no history of psychiatric or cognitive disorders; (3) no participation in similar MI programs; and (4) having no communication problems such as sight or hearing impairment. Unwillingness to stay in the study and admission to hospital during the study were considered exclusion criteria.
Measures
Demographic data were collected via questionnaire and included age, gender, occupational status, education level, marital status, duration of diabetes and type of medications. The Perceived Self-Efficacy Scale (SES), developed and validated by Naderimagham et al (2013) and Noroozi and Tahmasebi (2014), was used to evaluate self-efficacy. This instrument consists of 17 items covering five domains: a diabetes-specific diet (3 items), physical activity (4 items), blood glucose self-monitoring (3 items), foot care (4 items), and smoking cessation (3 items). The items in the SES are scored based on a five-point Likert scale (1=Completely disagree; 5=Completely agree), giving a total possible score range of 17–85. In the present study, we calculated the mean scores in this questionnaire. Four weeks after the intervention was completed, all participants completed the SES questionnaires again.
Intervention
The first author obtained permission from the Ethics Committee of Urmia University of Medical Sciences in Iran (IR.UMSU.RCC.1395.132). The first author explained to participants the purpose of the research and assured them their privacy and the confidentiality of their personal information. In addition, the participants signed an informed consent form and were notified of the voluntary nature of enrollment in the study.
The study protocol is outlined in Figure 1. After participants completed the questionnaires, they were randomly allocated to the intervention and control groups. Participants in the control group received local routine diabetes care, including three education sessions over the course of a week in the Urmia Diabetes Association. Each session lasted 1.5 hours, equating to 4.5 hours a week.

Participants in the intervention group received MI in addition to the routine education received by the control group. The intervention group was divided into three subgroups of 10 participants, for the purpose of delivering the group-based MI sessions. The MI sessions were delivered by the third researcher, who had previous experience regarding the MI method and had attended training in this regard. The session content related to diabetes-specific dietary habits, physical exercise, blood glucose monitoring, foot care and smoking cessation, and followed the structure outlined in Table 1, based on Miller and Rollnick (2012). The intervention was implemented in five sessions (two sessions of 30–45 minutes’ duration per week).

The content of the MI sessions was clear and provided based on the education level of the participants so that they could comprehend the teachings. The third researcher initiated the first MI session by introducing himself to the participants and creating a friendly atmosphere. The researcher was not allowed any prejudice, views or knowledge to affect his classroom behaviour while he remained focused throughout the sessions.
MI consists of four principles, including:
1. Expressing empathy (informing participants about their abilities and acceptance, reflective listening, and seeking to understand the person’s feelings and perspectives without judging or labeling).
2. Creating conflict (demonstrating the risks and severity of the effects of diabetes that participants might not acknowledge).
3. Rolling with resistance (reflective listening to the failures of participants).
4. Supporting self-efficacy (evaluating the past successes of participants and highlighting their abilities/achievements).
Four weeks after the intervention finished, once the questionnaire had been repeated, the MI sessions were offered to the control group.
Data analysis
Analysis was performed on 60 participants who completed the baseline and follow-up assessments. The Shapiro–Wilk test was used to determine the normal distribution of the data. Data were analysed using SPSS software version 23 (IBM Corp., Armonk, NY, USA). The descriptive (mean, standard deviation, number and percentage) and inferential (independent t-test, paired t-test, chi-squared test and analysis of covariance [ANCOVA]) statistics were used to analyse the data. A P-value of <0.05 was considered significant.
Results
There was no significant difference between the intervention and control groups regarding demographic characteristics (Table 2). Thus, it could be claimed that the research groups were homogeneous in terms of demographic characteristics.

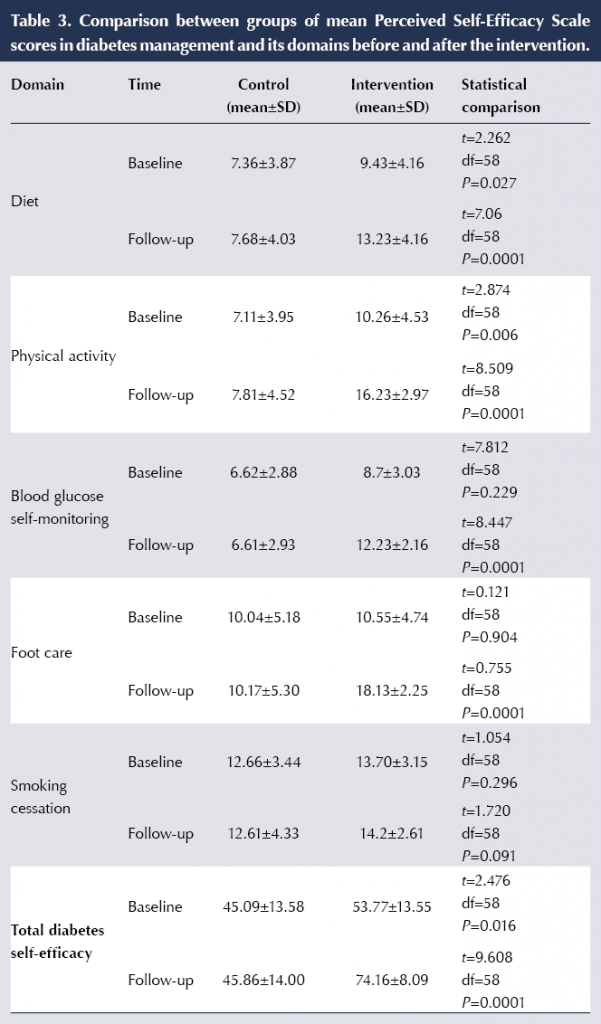
The independent t-test showed significant differences in mean scores for diet, physical activity, blood glucose self-monitoring, foot care and total self-efficacy between the intervention and control groups before and after the intervention (Table 3). No significant difference was observed between the groups in smoking cessation score either before or after the MI sessions.
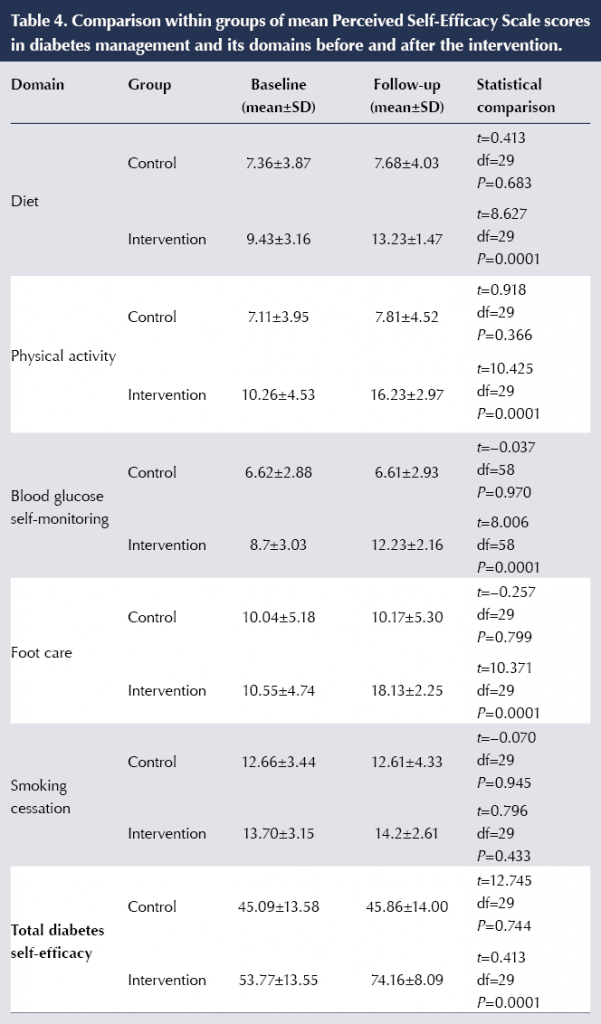
Compared with baseline, at 4 weeks’ follow-up the intervention group had significant increases in mean scores for diet, physical activity, blood glucose self-monitoring, foot care and total self-efficacy, but not smoking cessation (Table 4). In contrast, the control group had no significant differences in scores for any of the SES domains or total score.
Comparing the changes in scores over the study period, the intervention group had significantly greater increases across all SES domains and total self-efficacy compared with the control group (Table 5).

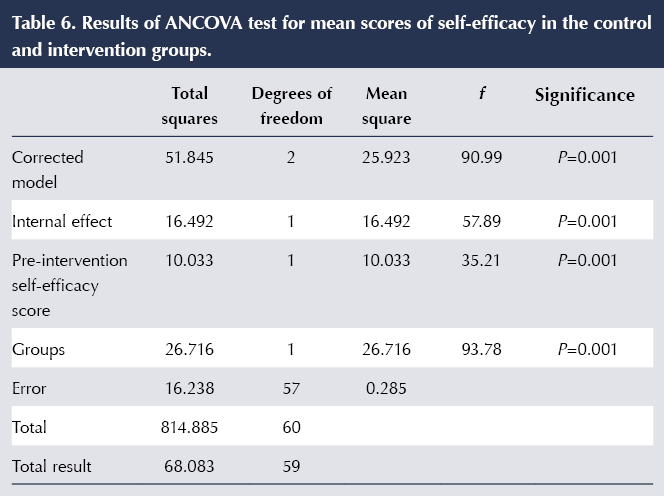
Because the mean total self-efficacy score was higher in the intervention group at the study start (Table 3), we used ANCOVA analysis to ensure that the significant between-groups difference in total self-efficacy score change at follow-up had been due to the MI educational approach. Following use of Levene’s test to confirm the homogeneity of variance between the two groups, the ANCOVA analysis confirmed that the effect of MI on total self-efficacy was significant (f=93.78; P<0.05; Table 6).
Discussion
The results of this study indicated no significant differences in demographic characteristics between the two groups. In other words, the study groups were homogeneous in terms of demographics, and any significant difference in the dependent variables could be attributed to the MI sessions at the end of the study.
Our findings also demonstrated that the MI approach positively influenced dietary self-efficacy in people with diabetes. These findings confirmed the hypothesis that MI is a more effective method in increasing the sense of self-efficacy of eating behaviour, as a predictor of success in weight loss programs (Ekong and Kavookjian, 2016). Baer (2015) hypothesised that low self-confidence in controlling eating behaviour, especially when experiencing negative emotions, is associated with symptoms of eating disorders.
Our results showed that physical activity could improve in people with diabetes after MI sessions, and confirm the results of Huffman et al (2021). A plausible explanation might be due to enhancing optimism and positive emotions, and reinforcing the self-care and self-management motivation of these individuals after MI sessions. In addition, the MI method could effectively enhance the sense of self-efficacy in the face of negative emotions, social pressure and physical discomfort situations, leading the individuals towards performing positive and enjoyable activities. The MI approach could create sustainable and relatively long-lasting changes in all mentioned parameters (Baer, 2015). Nowadays, experts consider physical exercise as the third central pillar of diabetes treatment, along with diet and medication, to decrease the disease burden and promote quality of life (Fujiwara et al, 2019). However, in contrast to our findings, Jansink et al (2013) showed that MI had no effect on improving physical activity. Hence, further studies seem necessary in this area.
Our results showed that the MI approach positively influenced self-monitoring of blood glucose in our participants with diabetes. In line with our findings, a recent systematic review showed that MI improves self-monitoring of blood glucose in people with type 1 diabetes (Dehghan-Nayeri et al, 2019). The basic principles of MI are reinforcing the sense of self-efficacy to the clients regarding all behavioural changes. Most of the MI techniques used in this research were exclusively related to this matter, such as evaluating commitment confidence, controlling temper in stimulating situations, participation in decision-making, supporting clients’ autonomy, eliminating bias and drawing attention to discuss change. In this respect, O’Halloran et al (2016) argued that the MI approach mostly emphasises self-efficacy, participation and improves psychosocial outcomes. Thus, it creates a strong sense of self-efficacy against temptations, therefore improving self-monitoring of blood glucose.
Our results indicated that the MI method positively influenced foot care, as has also been demonstrated in a recent US study (Celano et al, 2019). The MI approach could improve practical care in patients by compensating for disabilities and regulating individual performance.
The MI method had no effects on participants’ smoking cessation self-efficacy in the current study. Most people with diabetes are hesitant to make lifestyle changes because they are undecided, not because they are resisting the changes or lack the willpower. A systematic review showed that MI had no effect on smoking cessation in people with diabetes (Ekong and Kavookjian, 2016). Smoking cessation is a complicated process that may require other tools and coping strategies beyond MI, such as social support and sharing of information, emotions and concerns (Granado-Font et al, 2018).
Effective diabetes control requires understanding of the condition and required treatment procedures, and inadequate knowledge regarding the disease control process may decrease patients’ self-confidence. MI has a positive impact on individuals’ self-efficacy by affecting their perceptions and increasing their mental involvement to understand their condition and learn to manage their problems independently. After MI sessions in our study, the mean total score of self-efficacy increased in the intervention group, thus confirming that the MI approach could positively influence the self-efficacy of people with diabetes. These findings are congruent with those of Walpole et al (2013), who evaluated the effects of MI on self-efficacy in adolescents, and of Dogru et al (2012), who reported an improvement in the self-management of people with diabetes after implementing the MI approach.
In other research, MI was provided in the form of video calls as diabetes self-management education, and the results showed a significant improvement in participants’ self-efficacy (Hawkins, 2010). Song et al (2014) showed that MI positively impacted the self-management of people with diabetes. In another study focusing on self-efficacy and chronic diseases, Ebrahimi Belil et al (2018) observed that increasing self-efficacy resulted in creating a sense of empowerment to perform personal tasks, reducing fear, enhancing stress management, improving social relationships and promoting self-management. According to Sheeran et al (2016), self-efficacy could directly affect health-related behaviors, as well as other cognitive determinants. Furthermore, it could be argued that individuals with higher self-efficacy have more prominent personal goals, expect better outcomes and consider the obstacles against self-management as challenges to be overcome, all of which ultimately increase their self-management.
Contrary to our results, two similar studies showed that MI had no considerable impact on the routine self-care of patients with type 1 and type 2 diabetes (Rosenbek Minet et al, 2011; Welch et al, 2011). The reason for this, however, could be the high attrition rates that occurred in both studies.
Study limitations
One of the limitations of our study was the small sample number of participants, which might impact the effect size and statistical power of the study. Conducting the study in a small region with a specific cultural background was another limitation. The cultural tendencies of individuals affect their learning abilities and implementation of the teachings. Therefore, it is suggested that further investigations be conducted in this regard with larger sample sizes and larger areas with various cultures, so that the effects of MI on diabetes management self-efficacy could be confirmed, and the results could be generalised with greater confidence.
The fact that participants’ total self-efficacy score was higher in the intervention group at the study initiation was another weakness of this study. However, the authors attempted to control for this with an ANCOVA statistics test.
Conclusions
Self-efficacy plays a crucial role in predicting self-care activities in people with diabetes. The current findings suggest that self-efficacy could be improved by implementing the MI approach and increasing the individuals’ motivation. The diabetes associations could implement the MI method and promote self-efficacy in people with diabetes to promote health and quality of life.
Funding
This study was financially supported by the Deputy of Research Council of Urmia Medical Science University.
Author Contributions
All authors (Masumeh Hemmati Maslakpak, Naser Parizad, Amir Ghahremani, and Vahid Alinejad) have actively participated in this study. Design of the study: MHM, NP, AG, VA; data collection: NP, AG; analysis and interpretation of data: MHM, NP, AG, VA; manuscript preparation: MHM, NP, AG; manuscript revision: MHM, NP, AG, VA. All authors read and approved the final manuscript before submission.
Acknowledgments
This article was extracted from a Master’s thesis in nursing. Hereby, we extend our gratitude to the authorities of the Urmia University of Medical Sciences, the staff of Bukan Diabetes Association, and all the patients who participated and helped us in this research project. We also wish to thank Rosemary Carter for her review of the manuscript and writing assistance.





New handbook for healthcare professionals aims to improve outcomes
21 Nov 2024