Elmarie Van Wyk, Paediatric Diabetes Dietitian at the Great Western Hospital, Swindon, has written two approved leaflets for the South West Children & Young People’s Diabetes Network, titled “Understanding Glycaemic Index” and “Glycaemic Index and Insulin Therapy”. The former explains what the glycaemic index/glycaemic load (GI/GL) is, as well as the differences between high-, medium- and low-GI foods. The second leaflet explains the principles of GI in more detail, as well as providing practical advice on how individuals can adjust their insulin therapy.
The leaflets came about as a result of a quality assurance project, which Elmarie and Dr Nikolas Daskas (Consultant Paediatrician) decided to embark on after feedback from a number of families who reported either that there had been a noticeable change in the behaviour of their child or that their child was having difficulty concentrating after they had consumed certain types of breakfast meals. This change in behaviour was also associated with a high blood glucose reading at morning break time in school, with accompanied hypoglycaemia before lunch. This could be explained by the mismatch of insulin working action and the glucose release of the high-GI foods (Figure 1). The team was concerned about the behavioural and cognitive effects as well as the overall glycaemic impact on the children during this time and wanted to see what practical steps could be taken to address the issue.
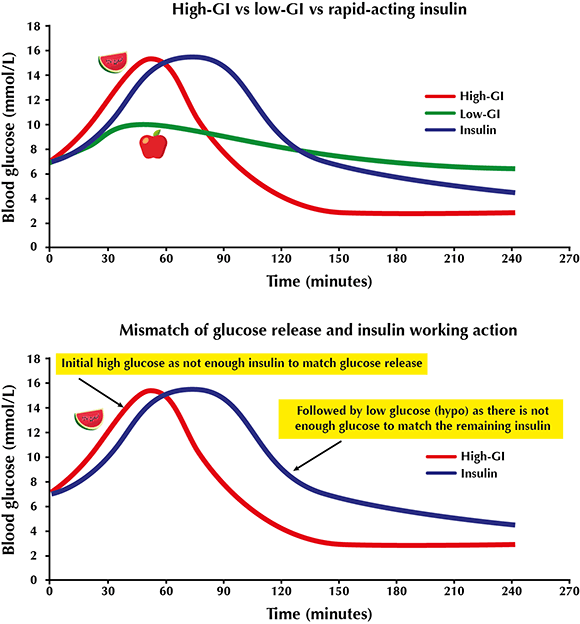
Figure 1. Mismatch of glucose release and Insulin working action.
The team’s research considered the management of postprandial hyperglycaemia in children with type 1 diabetes on multiple daily injections (MDI). The project was sponsored by Abbott, who provided a Freestyle Libre Handset and sensor for a two-week period. The main aims of the project were to gain a better understanding as to what happens with a child’s blood glucose levels after eating a high-GI breakfast; to be able to safely advise how much additional insulin (if any) is needed for high-GI breakfast foods in order to improve post-meal highs whilst avoiding hypoglycaemia; and to determine how long before breakfast one needs to inject to improve glycaemia in these circumstances.
As a result of this study and other evidence, the Glycaemic Index and Insulin Therapy leaflet was produced. It offers advice both to those on MDI and to those on pump therapy. It recommends what stage to inject insulin and offers guidance around giving a split/dual-wave bolus for high-GI food. Injecting rapid-acting insulin earlier with high-GI foods creates a much better match between insulin and glucose release.
The project has also raised a discussion around when GI/GL should be raised with families and what ongoing education needs to take place. Rather than focusing too much on the numerical issues of GI/GL, which can be fairly demanding, it is recommended that families are given the message about recognising the importance of healthy eating, including eating lean protein, soluble fibre, five fruit and vegetable portions a day, and including a low-GI food in each meal.


