The previously recognised high prevalence of type 2 diabetes in Asian people at lower BMI than in white people prompted the World Health Organization and NICE to recommend using a BMI of 27.5 kg/m2 to identify obesity and high cardiometabolic risk in South Asian and Chinese people, compared with a BMI of 30 kg/m2 for white individuals. However, as type 2 diabetes prevention is achievable with lifestyle or drug therapy in those at high risk, and early diagnosis and tight control of type 2 diabetes can provide long-term benefits, it is important to understand when to commence surveillance in non-white ethnic groups.
This large, longitudinal, population-based cohort study reviewed electronic records for nearly 1.5 million people in the Clinical Practice Research Datalink, linked to Hospital Episodes Statistics in secondary care, to identify those who developed type 2 diabetes over a median 6.5 years’ follow-up. Within this UK-based cohort, nearly 76,000 people were South Asian (5.2%), nearly 50,000 were Black (3.4%), around 11,000 were Chinese (0.7%) and 2764 were Arab (0.2%), with the remaining 90.6% Caucasian.
Overall, 6.6% of the cohort developed type 2 diabetes during the 6.5 years of follow-up. The median age at diagnosis was 67 years in Caucasians, 55 years in South Asians, 54 years in Black people, 60 years in Chinese people and 56 years in Arab people.
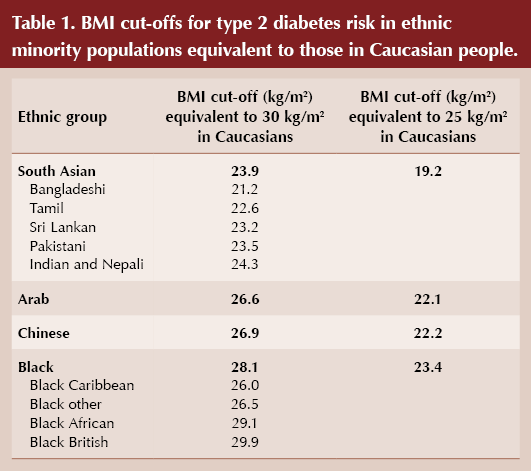
The authors calculated the equivalent age- and sex-adjusted incidence of type 2 diabetes at BMIs of 30 kg/m2 and 25 kg/m2 (the thresholds for obesity and overweight in the white population), and used these to identify BMI cut-offs for obesity and overweight for other ethnic groups, as shown in Table 1.
The BMI cut-offs proposed for Bangladeshi groups, as an example, are very low and, if implemented, would have a significant impact on UK services. However, helping people to understand the implications of their BMI on diabetes risk could motivate behaviour change in this particularly high-risk group.
Explaining the difficulties in calculating ethnicity-specific BMI cut-offs based on previous data, the authors identify limitations with previous studies, which used type 2 diabetes prevalence rather than incidence data, had small sample sizes, used surrogate markers and self-reported data, and included fewer ethnic groups.
The authors conclude that their data support revision of the UK BMI thresholds used to identify obesity and trigger action to prevent type 2 diabetes in people from non-white ethnic groups, to ensure they receive early surveillance to help prevent type 2 diabetes. However, these cut-offs only apply to the UK and the authors also call for identification of additional large data sets which would support complete revision of ethnicity-specific cut-offs in other countries. Furthermore, different cut-offs may be required if exploring the risk of cardiovascular disease or all-cause mortality rather than type 2 diabetes.
Since access to weight management services and surveillance for type 2 diabetes risk is usually limited by BMI thresholds, it is hoped that revising these cut-offs downwards for different ethnic groups would facilitate access to weight management services and earlier screening, prevention and diagnosis of type 2 diabetes.
Click here to read the study in full.





Jane Diggle discusses emotional health and diabetes distress, and offers some tips for discussing this in our consultations.
11 Nov 2025