Key studies
|
 |
Dapagliflozin improves renal outcomes in people with CKD, irrespective of diabetes status
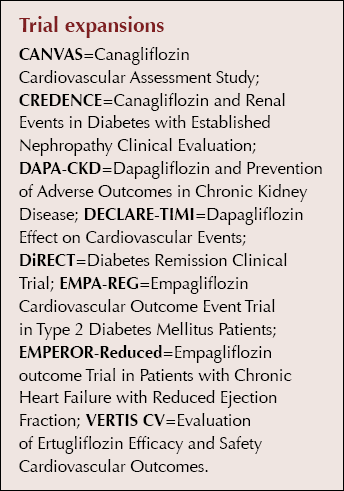
Results of the DAPA-CKD study of dapagliflozin for the treatment of chronic kidney disease (CKD) were presented, showing that the sodium–glucose cotransporter 2 (SGLT2) inhibitor significantly reduced CKD progression and mortality, irrespective of whether participants had type 2 diabetes or not. A brief summary of the findings is provided here; however, more in-depth analysis is available in the author’s report for Diabetes Distilled.
A total of 4094 people with CKD (estimated glomerular filtration rate [eGFR] 25–75 mL/min/1.73 m2 and urinary albumin:creatinine ratio (UACR) 23–565 mg/mmol) were randomised 1:1 to once-daily dapagliflozin 10 mg or placebo, in conjunction with standard care including a renin–angiotensin system blocker. The trial was ended early, after a median follow-up of 2.4 years, because of clear evidence of efficacy.
The primary outcome (a composite of ≥50% eGFR decline, end-stage renal disease or death from cardiovascular or renal causes) occurred in 9.2% versus 14.5% of the dapagliflozin and placebo groups, respectively (hazard ratio [HR], 0.61; 95% confidence interval [CI], 0.51–0.72). Each component of the primary outcome was significantly reduced in the dapagliflozin group. The benefits were consistent in both people with type 2 diabetes and those without.
All pre-specified secondary outcomes were significantly improved in the dapagliflozin group. Death from any cause occurred in 4.7% versus 6.8% in the two groups (HR, 0.69; 95% CI, 0.53–0.88). The number needed to treat to avoid one primary endpoint was 19.
Adverse and serious adverse event rates were similar in the two groups. Diabetic ketoacidosis (DKA) was not observed in any participant in the dapagliflozin group, and neither DKA nor severe hypoglycaemia was observed in any participants without type 2 diabetes.
Renoprotective effects for an SGLT2 inhibitor were previously shown in the CREDENCE study of canagliflozin. The present findings extend these benefits to people without type 2 diabetes. They also demonstrate that dapagliflozin is both safe and renoprotective when initiated in people with an eGFR as low as 25 mL/min/1.73 m2.
The full study results were simultaneously published in the New England Journal of Medicine. Click here to access.
VERTIS CV: Additional renal data and meta-analysis of SGLT2 inhibitor data
The key cardiovascular outcomes from the VERTIS CV study were presented at the American Diabetes Association’s Scientific Sessions earlier in 2020. While ertugliflozin achieved its primary endpoint of non-inferiority for major adverse cardiovascular events (MACE; cardiovascular death, non-fatal myocardial infarction and non-fatal stroke) versus placebo, neither the primary nor the secondary endpoints were significantly superior, raising questions about whether the benefits of SGLT2 inhibitors observed in other cardiovascular outcomes trials (CVOTs) could be truly seen as class effects.
At EASD, additional renal data were presented, comparisons between the outcomes of the different SGLT2 inhibitor CVOTs were reviewed and a meta-analysis of data from the four SGLT2 inhibitor trial programmes was presented.
Renal data
VERTIS CV was a CVOT; therefore, participants had a renal risk profile typical of those in other CVOTs; that is, <10% were deemed to be at high or very high renal risk as per KDIGO (Kidney Disease Improving Global Outcomes) classification. The original renal secondary outcome was a composite of renal death, ESRD (dialysis or transplant) or doubling of serum creatinine. This occurred in 19% fewer people treated with ertugliflozin 5 mg or 15 mg compared with placebo, but neither the composite nor its individual components were significantly reduced. Results of a number of other prespecified exploratory kidney endpoints were presented. Compared with placebo, the ertugliflozin group had a significant 34% reduction in a modified composite renal outcome (sustained 40% reduction in eGFR, ESRD or renal death), driven largely by reduced risk of a sustained 40% reduction in eGFR. Further exploratory analyses of subgroups demonstrated small decreases in albuminuric group progression (normal to microalbuminuric to macroalbuminuric) and higher rates of regression in those treated with ertugliflozin versus placebo. Median eGFR over time showed the typical initial dip seen with SGLT2 inhibitor treatment and then remained relatively constant, close to baseline level, over the course of the study, with a 2.55 mL/min/1.73 m2 difference between the groups, favouring ertugliflozin, by the end of the study. As expected, there was a trend towards increased differences between the groups depending on baseline albuminuria, with greater reductions in UACR in those with macroalbuminuria versus microalbuminuria or normal albuminuria.
SGLT2 inhibitor CVOTs compared
It is important to take into account the differences in the groups recruited to the individual SGLT2 inhibitor CVOTs as the populations had different cardiovascular and renal risk, and this will influence outcomes. All those recruited to the VERTIS CV trial had established atherosclerotic cardiovascular disease (ASCVD), as in the EMPA-REG study of empagliflozin. In a comparison presented at the conference, MACE was explored in those with and without ASCVD at baseline in each of the four CVOTs, and there was no evidence of significant benefit of ertugliflozin in those with ASCVD (the study population) or in those without ASCVD in the DECLARE-TIMI (dapagliflozin) and CANVAS (canagliflozin) programmes. However, when hospitalisation for heart failure (HHF) was examined across the trials, there was a consistent significant benefit versus placebo in each study and the meta-analysis demonstrated an overall significant 32% reduction, with no heterogeneity across the individual trials. Onset of benefit was demonstrated very early after treatment was commenced.
Exploring the prioritised renal outcomes for the individual SGLT2 inhibitor studies, ertugliflozin did not achieve a significant benefit in VERTIS CV, as discussed above (Table 1). However, if a sustained 40% reduction in eGFR was used in the composite renal endpoint, all four trials achieved significant reductions, and when these were pooled in the meta-analysis there was no heterogeneity between trials.
Summing up the implications of VERTIS CV for clinical practice, senior investigator Darren McGuire (UT Southwestern Medical Center, Dallas, TX, USA) concluded that the trial achieved its primary endpoint of non-inferiority for MACE versus placebo in people with type 2 diabetes and ASCVD, with no significant new adverse events identified. Meta-analysis confirms the recommendations to prioritise use of SGLT2 inhibitors for people with type 2 diabetes with or at high risk of cardiovascular and renal complications.
The full results from the VERTIS CV trial were published in the New England Journal of Medicine to coincide with the EASD symposium. Click here to access.
Once-weekly insulin: Phase 2 clinical trial
This 26-week, randomised, double-blind, phase 2 trial compared the efficacy and safety of two basal insulin analogues – once-weekly insulin icodec versus once-daily insulin glargine U100, in people with type 2 diabetes.
A total of 247 insulin-naïve people with type 2 diabetes treated with metformin and/or a dipeptidyl peptidase-4 (DPP-4) inhibitor were randomised to once-weekly icodec plus once-daily placebo, or to once-daily glargine plus once-weekly placebo. Insulin icodec was started at a dose of 70 units per week (10 units per day for insulin glargine) and both insulins were then adjusted in a treat-to-target-glycaemia approach (which had to be on a weekly basis for both groups to meet regulatory requirements).
At 26 weeks’ follow-up, mean HbA1c reduced from a baseline of around 64 mmol/mol (8.0%) by more than 11 mmol/mol in each group, and the authors concluded that the two agents had a similar glucose-lowering efficacy. There was an improvement in the mean of the 9-point patient-measured blood glucose profile with icodec compared to glargine, and those in the icodec group spent around an extra 78 minutes per day in the tight glycaemic range of 3.9–7.8 mmol/L compared with those in the glargine group, which may translate into clinically significant benefits. Participants in the study required a mean daily (or equivalent) insulin dose of 33 units of icodec or 41 units of glargine; however, the difference in insulin dose did not translate to a difference in weight gain. This will be explored further in future studies.
Hypoglycaemia rates were low. Mild hypoglycaemia (blood glucose <3.9 mmol/L) was more common with icodec (5.09 vs 2.11 events per person-year of exposure for icodec and glargine, respectively; rate ratio, 2.42); however, the incidence of clinically significant (blood glucose <3.0 mmol/L) or severe hypoglycaemia (that requiring third-party assistance) were low and similar in the two groups. There were no unexpected safety findings and adverse events were mostly mild, and none of the serious adverse events were adjudicated to be due to the study drugs.
This was a small phase 2 trial with a new once-weekly insulin currently in development by Novo Nordisk, and was not powered to detect significant differences between treatments for any endpoints. Many people with type 2 diabetes are reluctant to start insulin. The authors hope an insulin that could be used once weekly, requiring only 52 instead of 365 injections per year, would improve acceptance and adherence, as has occurred with once-weekly compared to daily GLP-1 RAs.
The full study results were simultaneously published in the New England Journal of Medicine. Click here to access.
Intermittent versus continuous very-low-calorie diet may be more achievable
Issa BG et al; Abstract 208
The MIDDAS (Manchester Intermittent vs Daily Dieting Diabetes App Study) pilot was designed to compare the feasibility and efficacy of an intermittent low-energy diet (ILED) versus a continuous low-energy diet (CLED) in people with obesity and type 2 diabetes. The study recruited people aged 18–75 years with HbA1c ≥48 mmol/mol (6.5%), BMI 27–50 kg/m2 (25–50 kg/m2 in high-risk ethnic groups) and type 2 diabetes of up to 8 years’ duration, including those on insulin (a group excluded from the DiRECT study). Those with an HbA1c ≥108 mmol/mol (12.0%) in the last 3 months were excluded.
The year-long study was divided into two phases. In the active weight loss phase, the CLED group (n = 40) followed an 800 kcal/day liquid diet, 7 days per week, for 8 weeks, followed by a 4-week food reintroduction phase (1000–1500 kcal/day). This was followed by a 40-week weight maintenance phase, in which participants followed a portion-controlled Mediterranean diet. The ILED group (n = 39) had a 28-week active weight loss phase (800 kcal liquid diet for 2 days a week, and portion-controlled Mediterranean diet for the other 5 days), followed by a 24-week maintenance phase (food-based 800 kcal diet twice per week and a portion-controlled Mediterranean diet 5 days per week). Participants could enter a relapse programme if they put on more than 2 kg of weight.
Metformin was continued but other medication was stopped completely in the CLED group, while medication with a risk of hypoglycaemia was omitted on low-calorie days in the ILED group. High-frequency remote support was provided from a multidisciplinary team, including a diabetes dietitian, diabetes nurse, exercise specialist and psychologist if appropriate (around half of participants), via the Oviva app and/or by telephone. The app allowed participants to log food intake, weight, blood glucose and activity, as well as receive communication from the team. The primary outcomes were uptake, retention, achievement of HbA1c <48 mmol/mol, and weight loss of ≥10% and ≥15%. Secondary outcomes were adherence, adverse events, changes in diabetes medications and use of the Oviva app, over the 1-year time frame. The study was designed to assess feasibility and efficacy but was not powered to assess differences between the groups.
Retention was good, with 69% of the ILED group and 75% of the CLED group completing the study. The CLED group lost more weight by 12 weeks (9.7%) but, due to weight regain, at 12 months the weight loss relative to baseline was similar in the two groups (6.0% and 5.4% in the CLED and ILED groups, respectively). Overall, 20% of both groups achieved ≥10% weight loss and around 5% achieved ≥15% weight loss. Although just over 40% of participants achieved an HbA1c <48 mmol/mol, this required less medication in the CLED group. Nine adverse events occurred in eight of the 79 participants, caused by gall bladder conditions, but none withdrew from the study.
This was a pilot study and the authors concluded that larger studies are needed to identify the impact of ILED versus CLED on additional parameters and outcomes.
In the DiRECT study, many participants found it difficult to spend 8–20 weeks without normal food and eating opportunities, and after 2 years an average of 40% of the weight lost had been regained despite ongoing intensive support and the opportunity to restart the very-low-calorie shakes during follow-up (Lean et al, 2019). The 800 kcal liquid diet and support used in DiRECT is currently being rolled out across 5000 people with type 2 diabetes across 10 areas of England. The MIDDAS pilot explored the feasibility and efficacy of an alternative way to use a very-low-calorie diet to achieve significant weight loss, including achieving this remotely, which is particularly relevant in the current COVID-19 environment.
LIBERATES: Using flash monitoring to improve glycaemic control post-MI
Heller SR (Chair); Symposium 11
Optimising blood glucose levels in people with type 2 diabetes post-myocardial infarction (MI) is important but can be challenging. The LIBERATES trial randomised 141 people with type 2 diabetes and new myocardial infarction, treated with insulin and/or sulfonylureas (SUs), to flash glucose monitoring or conventional fingerprick self-monitoring of blood glucose (SMBG), starting within 5 days of their MI and continuing for 3 months. The primary outcome was time in range (TIR) 3.9–10 mmol/L during the final 14 days of the study, and prespecified secondary and exploratory outcomes included time spent in hypoglycaemia, HbA1c, quality of life measures, major adverse events and cost-effectiveness.
At baseline, 55% of participants were on insulin and the remainder were on SUs; 86% were treated with additional glucose-lowering medications, and the use of insulin and SUs was similar between the groups. During days 76–90 there was a small increase in TIR in the flash monitoring group, but this was not significant. However, when data from days 16–30 were explored, those on insulin had a significant additional 3 hours per day in target range in the flash glucose monitoring versus SMBG group.
There was a trend towards less time in hypoglycaemia in insulin- and SU-treated flash users at days 16–30, and there was a significant reduction of more than 1 hour per day across the overall intervention group (insulin and SU) versus controls at days 76–90; this increased to around a 2-hour redution in SU recipients in the flash monitoring versus SMBG group. There was no difference in HbA1c at day 90 between flash monitoring and SMBG; however, HbA1c fell by 7 mmol/mol in both groups compared with baseline.
When quality of life was explored, there was increased awareness of hyper- and hypoglycaemia in those using flash glucose monitoring, with higher scores compared with the SMBG group in terms of convenience, flexibility and understanding of diabetes. No severe hypoglycaemia was seen in the intervention group, compared to 2.8% in controls, and there were fewer deaths (2.9% vs 4.2%) in the flash monitoring group. MACE data are still being evaluated.
Early-onset type 2 diabetes twice as common in South Asian and African–Caribbean populations
Ranchagoda JD et al; Abstract 153
Type 2 diabetes developing in early adulthood versus later in life, which is becoming more common in the UK, results in accelerated risk of complications and early mortality. In a cross-sectional study of nearly 1.5 million GP records across Northwest London, researchers at Imperial College London and Imperial College Healthcare Trust analysed the prevalence of early-onset adult type 2 diabetes in diverse ethnic groups, and explored the links between BMI and age at diabetes onset. Early onset was defined as age 18–44 years at diagnosis.
The prevalence of type 2 diabetes at all ages was 6.5% overall, but it was 3.4% in white people compared to 10.1% in South Asians and 8.3% in African–Caribbean people. The proportion with early-onset diabetes was 15.7% amongst white people, with a peak age at diagnosis of 55–64 years (28.8% of diagnoses). In contrast, 30.7% of cases amongst South Asians were diagnosed at age 18–44 years, with a peak age at diagnosis of 45–54 years (around a third of diagnoses). Among African–Caribbeans, 25.8% had early-onset type 2 diabetes and, like the South Asian group, the most common age range at diagnosis was 45–54 years, again with around 30% being diagnosed in that decade.
Those with an early-onset type 2 diabetes diagnosis had significantly higher BMI across all ethnicities than those diagnosed at 55–79 years, and the BMI for both groups was highest in white people, lower amongst African-Caribbeans and lowest amongst South Asians.
This doubling of the prevalence of young-onset type 2 diabetes in those of South Asian and African–Caribbean ethnicities compared to white individuals should prompt us to be more vigilant in searching out these people, so that they can have prompt treatment and be encouraged to aim for tight control in the hope that we can reduce the impact of untreated diabetes.
UK Biobank study
Young KG et al; Abstract 331
HbA1c screening of people aged 40–70 years could identify those with type 2 diabetes two years earlier, according to a study of more than 200000 UK Biobank participants. Overall, 1% of participants (n = 2174) had undiagnosed type 2 diabetes (HbA1c ≥48 mmol/mol [6.5%]) at baseline testing. Reviewing electronic primary care records, the median time to diabetes diagnosis was 2.3 years and 23% of this group had still not received a diagnosis 5 years later. Those with HbA1c ≥48 mmol/mol had a higher BMI (31 vs <27 kg/m2) and were slightly older overall.
Presenting the data, Katie Young (University of Exeter) concluded that further research is needed to fully clarify the impact on diabetes-related complications, although no significant impact was demonstrated in this study.
UK Biobank data resulted in many additional studies presented at the conference, and this rich source of data is likely to continue to inform our practice.
Using UK data to model lost life-years in people with diabetes
Stedman M et al; Abstract 265
A modelling study on the UK population, using data from the National Diabetes Audit and the Office of National Statistics by a team from Salford University, explored the number of life-years likely to be lost to diabetes in the current population. This demonstrates that the “average” person with type 1 diabetes, now aged 42.8 years, will survive for an additional 32.6 years, compared to 40.2 years in someone without diabetes of the same age, resulting in an average of 7.6 years of life lost. In an “average” person with type 2 diabetes, currently aged 65.4 years, the average life expectancy would be 18.6 years compared with 20.3 years in someone of the same age without diabetes: a loss of only 1.7 years. Women were likely to lose more life-years than men.
This modelling suggests that diabetes would result in a total of 6.4 million future life-years lost when the current population is considered. For both those with type 1 and type 2 diabetes, it was estimated that each year with an HbA1c >58 mmol/mol (7.5%) results in a loss of around 100 life-days, and the authors hope that this may help motivate both clinicians and people with diabetes to aim for tighter glycaemic control.
The full report is available in Cardiovascular Endocrinology & Metabolism. Click here to access.
UK glucose-testing protocol supports flying by insulin-treated commercial pilots
Garden GL et al; Abstract 754
Previously, use of insulin barred people with diabetes from many “safety-critical” occupations, including flying commercial aircraft. In 2012, the UK Civil Aviation Authority began certifying carefully selected insulin-treated pilots on the basis of a rigorous blood glucose testing protocol and reviews, and pilots in Ireland and Austria are now using the same protocol.
Gillian Garden (University of Surrey) presented the outcomes of an observational study of blood glucose data from more than 22000 hours of flying by 49 pilots (84% with type 1 diabetes) who had been granted medical certification to fly both short- and long-haul commercial aircraft while following this glucose monitoring protocol. More than 97% of readings taken according to the protocol prior to and during flights were within the green range (5–15 mmol/L), with only 0.12% of the readings within the low red range (<4 mmol/L). Out-of-range readings improved during the duration of the protocol use. No episodes of incapacity or safety problems were reported during the 7.5 years of the study, and the protocol was found to be feasible, practical and easily understood. All results were verified by the co-pilot and spoken into the data voice recording. Responding to questions, the lead author confirmed that, following any change in type of insulin, flying is barred for 3 months and that other rigorous safety reviews must also be undertaken. The authors concluded that these data may be useful in decision-making when considering other safety-critical occupations. Data from concomitant use of continuous glucose monitoring (CGM) devices, as well as the fingerprick sampling, have been collected in parallel, and it is hoped that these results will ultimately permit use of CGM as the preferred monitoring method. The full report is available in Diabetes Care. Click here to access.






Poster abstract submissions are invited for the 21st National Conference of the PCDO Society, which will be held on 19 and 20 November.
10 Apr 2025