I was prompted to write this article after hearing a dietitian extol the virtues of the Eatwell Guide to an audience of primary care colleagues who wished to update their knowledge on best practice dietary advice for people with type 2 diabetes. In the dietitian’s defence, the Eatwell Guide represents current conventional thinking around what constitutes healthy eating for both the general population in the UK and for people with type 2 diabetes.
Dietary support and advice is an essential part of the package of care that we offer within primary care. In recent years, however, the mainstream recommendations have been increasingly challenged, with one critic going as far as suggesting: “There is an epidemic of misinformed doctors and patients” (Malhotra, 2019).
Daily, we are bombarded with often confusing and contradictory claims about the virtues and sins of certain food. In this article, I explore the differing views of what constitutes healthy eating for people with type 2 diabetes, what makes sense to me and how I have applied this in my clinical practice.
The public health message
National guidance on healthy eating in the UK is depicted in the Eatwell Guide, which shows what proportion of a healthy, balanced diet should come from each of the main food groups (Public Health England [PHE], 2016). It recommends that at least one third of food intake is based on starchy carbohydrate (albeit the wholegrain or higher fibre versions, with less added fat, salt and sugar) and that we should strive to eat at least five portions of fruit and vegetables a day. Consequently, it recommends that >50% of daily calorie intake should come from starchy foods, fruit and vegetables.
A whole host of emotional, psychological and social factors drive us to eat (or not), but, from a purely physiological perspective, we eat to survive – to obtain nutrients and energy to fuel all bodily functions. Essential nutrients are those that are required for survival, but which cannot be produced by the body. They must, therefore, be obtained from a dietary source. There are essential fats and essential proteins, but no essential carbohydrates.
According to the Institute of Medicine of the National Academies (2005): “The lower limit of dietary carbohydrate compatible with life apparently is zero…”. There is, however, a commonly held belief that we need to consume at least 130 g of carbohydrate per day, a figure derived, in part, from the brain’s glucose requirement. Typically, carbohydrate does form the main energy source for the body and represents the most metabolically efficient source for the production of energy. If there is insufficient carbohydrate in the diet to produce enough glucose to meet the body’s energy requirements, the shortfall can be met by a number of other metabolic processes, including glycogenolysis (the breakdown of stored glycogen into glucose) and gluconeogenesis (the synthesis of glucose from non-carbohydrate sources, namely amino acids from protein and glycerol from fat).
When carbohydrate intake is significantly restricted (to around 20–50 g daily), glycogenolysis in the liver and muscles releases glucose for energy. After a couple of days, these stores will be fully depleted and the body begins to break down fats from the diet and stored body fat to produce energy. The fatty acids produced cannot cross the blood–brain barrier, so must be broken down into ketone bodies in a process called ketogenesis before being transported into the brain to provide the energy it requires. Under normal conditions, the concentration of plasma ketone bodies is very low (<0.3 mmol/L), but this can rise to 7–8 mmol/L during periods of nutritional ketosis (Health Engine, 2019).
It is important to note that this is very different from diabetic ketoacidosis (DKA), a very dangerous and potentially life-threatening condition most likely to occur in type 1 diabetes as a result of severe insulin deficiency. In this situation, ketone levels can exceed 20 mmol/L (Paoli, 2014) and be accompanied by symptoms that include breathlessness, fatigue, dizziness, nausea and extreme thirst. It can lead to coma and eventually death. It is important to be aware that there have been rare occurrences of “euglycaemic” DKA (i.e. DKA without marked hyperglycaemia) in individuals with type 1 or type 2 diabetes taking sodium–glucose cotransporter-2 (SGLT2) inhibitors (Brown, 2018) but, again, this is entirely different to nutritional ketosis.
Is there an ideal macronutrient ratio?
The food we eat is made up of macronutrients (carbohydrate, fat and/or protein) and various micronutrients (vitamins and minerals). Most foods are a combination of all three macronutrients, but is there an ideal macronutrient ratio for optimum health and is it any different for a person with type 2 diabetes? This is the million-dollar question for which, as yet, we have no clear answer.
According to the American Diabetes Association (ADA, 2018), “Evidence suggests that there is not an ideal percentage of calories from carbohydrate, protein and fat for all people with diabetes.” The consensus within this report is that the macronutrient distribution should be agreed on an individual basis, taking account of current eating patterns, preferences and metabolic goals.
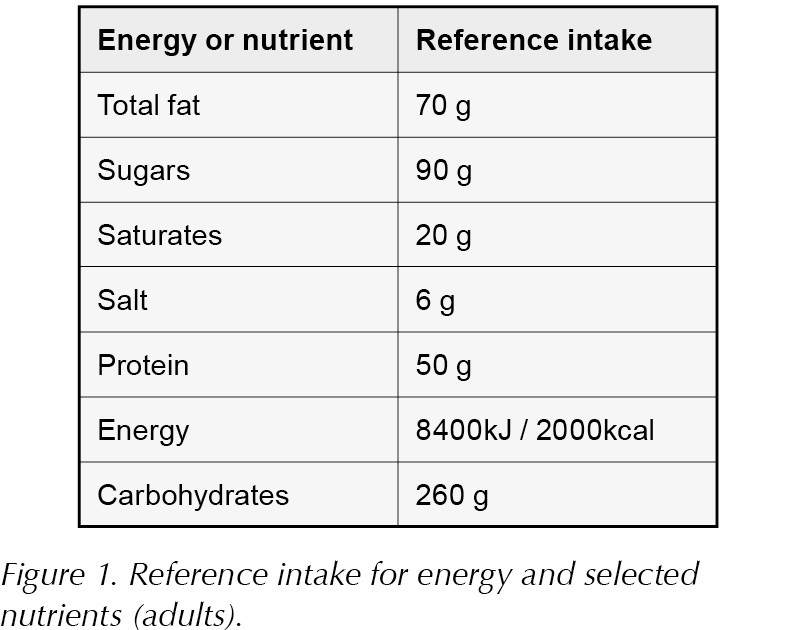
In the UK, however, reference intake tables (as illustrated in Figure 1) are commonly used to communicate a recommended maximum nutrient intake for the general adult population. The values shown reflect the Government’s dietary recommendations (PHE, 2016).
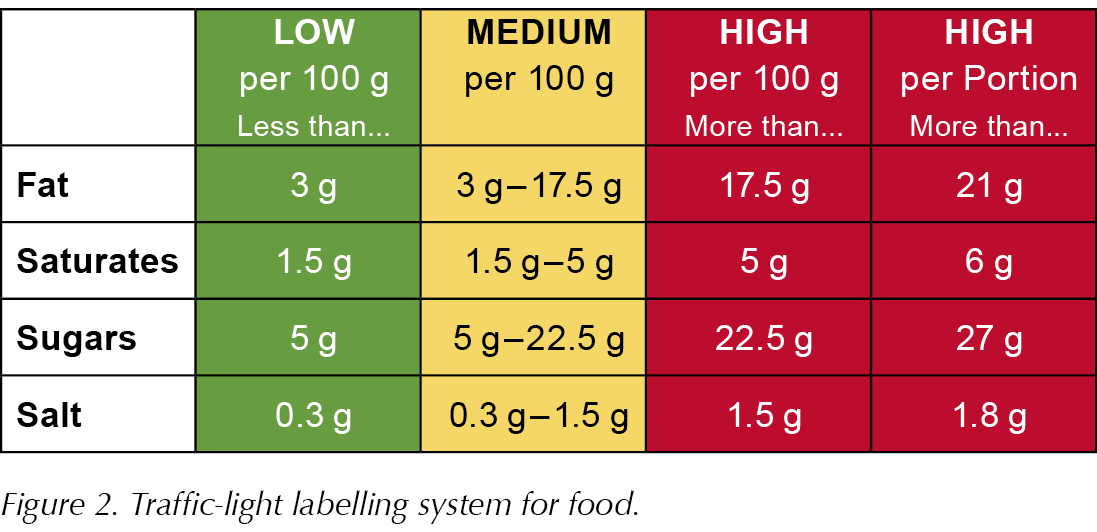
A traffic-light system (Figure 2) appears on food labels to help consumers understand the nutritional content of food products and more easily make healthier choices.
The UK Government issued dietary guidelines in 1983 that closely followed those issued in the US a few years earlier. The emphasis was, and continues to be, on reducing saturated fats and dietary cholesterol.
In the 1950s, Ancel Keys, an American researcher and physician, described the correlation between heart disease and saturated fat, which subsequently shaped public health dietary recommendations across the nations for decades. The so-called diet–heart hypothesis has been questioned over the years. In 1972, John Yudkin, a British scientist, proposed that sugar, not fat, was the greater danger to health. At the time, his findings were ridiculed, as the public health message continued to focus on reducing fat to improve health. As journalist Ian Leslie points out, consumers followed the advice and “replaced steak and sausages with pasta and rice, butter with margarine and vegetable oils, eggs with muesli, and milk with low-fat milk or orange juice” (Leslie, 2016). Obesity rates after World War II remained at a low level (6%) until the mid 1980s when, coinciding with the national dietary recommendations, they rose rapidly.
Is the nation following the dietary recommendations?
The National Diet and Nutrition Survey (NDNS) is a continuous cross-sectional survey designed to assess the diet, nutrient intake and nutritional status of a representative sample of around 1000 people per year from the general population living in private households in the UK (PHE, 2019). The results provide the evidence base for policy development and enable progress towards public health nutrition objectives to be tracked. In 2014, the NDNS showed that, on average, adults in the UK were eating 383 kcal below the recommended daily amount, while food energy from total fat consumption was just below the recommended 35%.
The latest figures, published in January 2019, have shown little change to total energy (calorie) intake or total fat consumption, but, overall, the UK population continues to consume too much sugar and saturated fat, and not enough fruit and vegetables, fibre or oily fish.
PHE (2016) recommends that we do not exceed 10% of daily calorie intake from saturated fat (men should eat no more than 30 g of saturated fat and women no more than 20 g). It has been suggested that most of our saturated fat intake comes from milk products (such as whole milk and cheese), cereal products and meat products. Interestingly, the top ten sources of saturated fat in the US are reported to be cheese, pizza, grain-based and dairy-based desserts, chicken dishes, processed meats, burgers, Mexican dishes, meat dishes and low-fat milk (National Cancer Institute, 2018). However, many of these are also high in carbohydrate, so reducing these “junk foods” would also reduce saturated fat.
Despite evidence supporting a reduction in total fat consumption in the population over the past 20–30 years, obesity rates have continued to rise. Protein consumption remains fairly constant at around 15% of total intake (Wardlaw and Smith, 2008), suggesting that attempts to reduce total fat intake have led to an increased intake of the remaining macronutrient – carbohydrate.
Not only is the population becoming fatter but, by association, type 2 diabetes prevalence is also rising rapidly. The Health Survey for England 2015 reported an increase in obesity prevalence from 15% in 1993 to 27% in 2015 (Moody, 2016). According to latest figures from Diabetes UK, 3.8 million individuals are diagnosed with diabetes (90% with type 2 diabetes), with a further 1 million unaware they have the condition, giving an estimated total of 4.7 million. This figure is expected to rise to 5.5 million by 2030 (Diabetes UK, 2018a).
This raises the question as to whether mainstream dietary advice is appropriate for people with diabetes. To understand this better, it is useful to remind ourselves of how the body utilises carbohydrates and where this goes wrong in type 2 diabetes.
Carbohydrate metabolism and type 2 diabetes
Carbohydrates are not inherently unhealthy – most individuals are able to handle a moderate amount of carbohydrate in their diet. Except for fibre, all types of carbohydrate – whether starchy or sweet, wholegrain or refined – are broken down into glucose in the gastrointestinal tract before being absorbed into the bloodstream. Glucose is the body’s preferred fuel source. Stimulated by the release of insulin, it is taken into cells throughout the body as fuel. Unused glucose is converted to glycogen and stored (mostly in the liver and muscles) but, once these stores are full, excess glucose is converted to fat for the long-term storage of energy.
Clearly, insulin has a vital role to play in glucose metabolism, but it also acts as a fat-storing hormone, as it inhibits the breakdown of adipose tissue. Carbohydrate intake stimulates insulin secretion far more than protein or fat. Jason Fung, a nephrologist and author of The Diabetes Code (2018) is convinced that type 2 diabetes is caused by the chronic overconsumption of carbohydrates stimulating the body’s insulin response.
Gary Taubes, author of Good Calories, Bad Calories: Fats, Carbs and the Controversial Science of Diet and Health (2007) and Why We Get Fat (2010) holds a similar view, describing obesity as “…not so much a disease of energy imbalance but one of fat accumulation caused by excess insulin, driven primarily by carbohydrate consumption”.
This underlying process is certainly in line with the twin-cycle hypothesis of the mechanisms that lead to type 2 diabetes proposed by Roy Taylor (2013). Professor Taylor explains how, over time, a person eats too much food and excess carbohydrates are converted into fat. This fat accumulates in the liver, muscles and tissues, as well as in the pancreas, leading to insulin resistance in which cells fail to respond normally to this hormone. Insulin is unable to suppress glucose production in the liver and, despite already raised blood glucose levels, even more glucose is released into the bloodstream. This, in turn, stimulates yet more insulin secretion from the pancreas, promoting more fat storage and a positively reinforcing vicious cycle that ultimately leads to type 2 diabetes.
Current guidance on healthy eating for people with type 2 diabetes
For people with type 2 diabetes, NICE recommends integrating dietary advice with other aspects of lifestyle modification, such as physical activity and weight loss. The emphasis is on encouraging the same balanced diet that is applicable to the general population; that is, high-fibre, low-glycaemic-index sources of carbohydrates (e.g. fruit, vegetables, wholegrains and pulses, which raise blood glucose levels slowly), low-fat dairy products and oily fish; and to control the intake of foods containing saturated and trans-fatty acids (NICE, 2015).
It recommends:
- Energy restriction to induce 5–7% weight loss.
- Dietary modification including:
– Reduced saturated fat intake (<10% total energy intake)
– Increased dietary fibre intake (>15 g/1000 kcal)
Information for the general public on the NHS (2018) website states that:
- Carbohydrates should be the body’s main source of energy in a healthy, balanced diet.
- The government’s healthy eating advice, illustrated by the Eatwell Guide, recommends that just over a third of your diet should be made up of starchy foods, such as potatoes, bread, rice and pasta, and over another third should be fruit and vegetables. This means that over half of your daily calorie intake should come from starchy foods, fruit and vegetables.
- People with diabetes should try to eat a healthy, balanced diet, as shown in the Eatwell Guide.
When the Eatwell Guide was introduced, several menu suggestions appeared alongside it. Dr Zoë Harcombe, a researcher, author, blogger and public speaker in the field of diet and health, who has openly criticised the Eatwell Guide, subsequently revealed that many of these menu suggestions were deficient in essential nutrients (particularly fat-soluble vitamins), had high levels of sodium and sugar, and represented on average 375 g of carbohydrate a day (Harcombe, 2016). This represents considerably more total carbohydrate than appears in the reference intake guide (the maximum recommended daily intake). Given that type 2 diabetes is characterised by an inability to utilise glucose adequately, it seems odd that this recommendation is based on the very food group that provides the main source of glucose.
Dietary recommendations from Diabetes UK
Diabetes UK still supports the Eatwell Guide as a resource for people with diabetes (Diabetes UK, 2017a). However, the advice on starchy carbohydrates did shift during 2015. In March of that year, it recommended “5–14 portions – one third of your diet should be made up of these foods [starchy carbohydrates], so try to include them in every meal”. Examples of a portion were given and included 2–4 tbsp cereal; 1 slice of bread; 2–3 tbsp rice, pasta, couscous, noodles or mashed potato; 2 new potatoes or half a baked potato; half a small chapatti; and 2–3 crispbreads or crackers. Two months later, however, the wording changed. These examples were removed and preferred starchy food options were listed as wholewheat pasta, basmati rice, brown or wild rice, granary bread and oat-based cereal, such as porridge or natural muesli. The recommended 5–14 portions changed to, “Try to have some starchy food, especially the wholegrain options, every day.”
Perhaps even more telling of the shift in advice towards reducing carbohydrate intake is the paragraph that reads: “Carbohydrates break down to glucose in the blood, so keep an eye on how much you eat. Depending on your diabetes treatment, and nutritional goals, you may be advised to:
- Estimate the amounts of carbs you are eating.
- Reduce the amounts of carbs you eat.
- Choose healthier sources.
- Spread your intake through the day.” (Diabetes UK, 2015)
In March 2018, Diabetes UK launched new nutrition guidelines for the prevention and management of diabetes (Diabetes UK, 2018b). Key messages include that one size does not fit all and that advice needs to be individualised. In line with current NICE guidance (2015), sustained weight loss of at least 5% in overweight people by reducing calorie (energy) intake and increasing energy expenditure is a priority. A Mediterranean-style diet or equivalent healthy eating pattern is recommended that includes:
- Reducing salt intake (<6 g/day).
- Eating two portions of oily fish each week.
- Eating more wholegrains, fruit and vegetables, fish, nuts and legumes (pulses).
- Eating less red and processed meat, refined carbohydrates and sugar-sweetened beverages.
- Replacing saturated fats with unsaturated fats, and limiting intakes of trans fatty acids.
- Limiting alcohol intake to <14 units a week.
- Aiming for at least 150 mins per week of moderate to vigorous physical activity, over at least 3 days.
The guidelines do not recommend the use of foods marketed specifically for people with diabetes. Nor do they support low-carbohydrate diets over other dietary approaches, but they do advocate greater carbohydrate awareness, including the recommendation to: “Offer individualised education to support people to identify and quantify their dietary carbohydrate intake, encourage low glycaemic index (GI) foods and consider reducing the total amount of carbohydrates.”
Diabetes UK does acknowledge that some people with diabetes may want to follow specific diets that may not be completely in line with the Eatwell Guide, but should still include foods such as fruit and vegetables, wholegrains, dairy, fish, pulses and nuts (as these foods have been shown to promote good health), and limit the intake of red and processed meat, sugary soft drinks, sugar-sweetened foods and other refined carbohydrates.
The role of low-carbohydrate diets
The increasing interest in low-carbohydrate diets may have been what prompted Diabetes UK (2017b) to publish a position statement on the subject that states:
- Low-carbohydrate diets can be safe and effective in the short term in managing weight, and improving glycaemic control and cardiovascular risk in people with type 2 diabetes.
- People who choose to follow a low-carb diet should be supported to make changes to relevant diabetes medications and to monitor blood glucose to reduce the risk of hypoglycaemia.
- Whether people choose to follow a low-carb diet or not, they should be encouraged to include foods with good evidence to support health. This includes fruit and vegetables, wholegrains, dairy, seafood, pulses and nuts.
- People should be encouraged to reduce their intake of red meat and processed meat, sugar-sweetened foods, particularly sugar-sweetened drinks, and refined grains such as white bread.
NHS England responded to the increasing public interest in low-carb eating in a blog entitled The truth about carbs, suggesting that, “While we should reduce the amount of free sugar in our diet, we should base our meals on starchy carbs, particularly the higher fibre varieties [because] there is strong evidence that fibre, found in wholegrain versions of starchy carbs for example, is good for our health” (NHS, 2018).
Sources of fibre include fruit, vegetables, cereals and pulses – foods that also tend to have a high carbohydrate content and may present a challenge for those opting to eat a low-carb diet. However, choices of these food types must be made carefully. Meeting the 30-g fibre intake that is recommended could mean eating 5 apples, 2 oranges and 3 pears – but that amounts to 143 g of carbohydrate (equivalent to 10 tablespoons of sugar!).
Certain wholegrain breakfast cereals are advertised as being high in fibre. In one such example, however, a 30-g serving has just 2.5 g of fibre, but 13 g of sugar (3 teaspoons). However, it is possible to meet the fibre intake recommendations by including lower-sugar fruits (such as berries), non-starchy vegetables (broccoli, kale and spinach), avocado, asparagus, celery, aubergine, seeds (flax, chia, hemp and sesame) and nuts (such as almonds). Providing there is adequate intake of these foods, reducing carbohydrate intake would not increase the risk of insufficient intakes of certain nutrients.
Is there an ideal amount of carbohydrate for type 2 diabetes?
There is no consistent and robust evidence to recommend the ideal amount of carbohydrate for a person with diabetes, as this will vary between individuals and will alter with circumstances. However, type 2 diabetes is a condition in which there is an inability to effectively metabolise carbohydrates and, by definition, a degree of “carbohydrate intolerance”.
The speed at which carbohydrates are converted to glucose is variable and may be affected by many factors, including glycaemic index, portion size, cooking methods, amount of processing, combining with other food types and physical activity. Carbohydrates raise blood glucose levels more than any other food group. Type 2 diabetes is a condition characterised by raised blood glucose levels and a primary treatment goal is to lower them to reduce the risk of associated complications.
Both fats and carbohydrates have been blamed for increasing a person’s likelihood of becoming overweight or obese. It remains a hotly debated topic, though recently the view that an excessive consumption of carbohydrate may be the main driver for obesity, and specifically for type 2 diabetes, has gained more traction. Alongside this, greater interest in low-carb eating has emerged.
Defining low carbohydrate
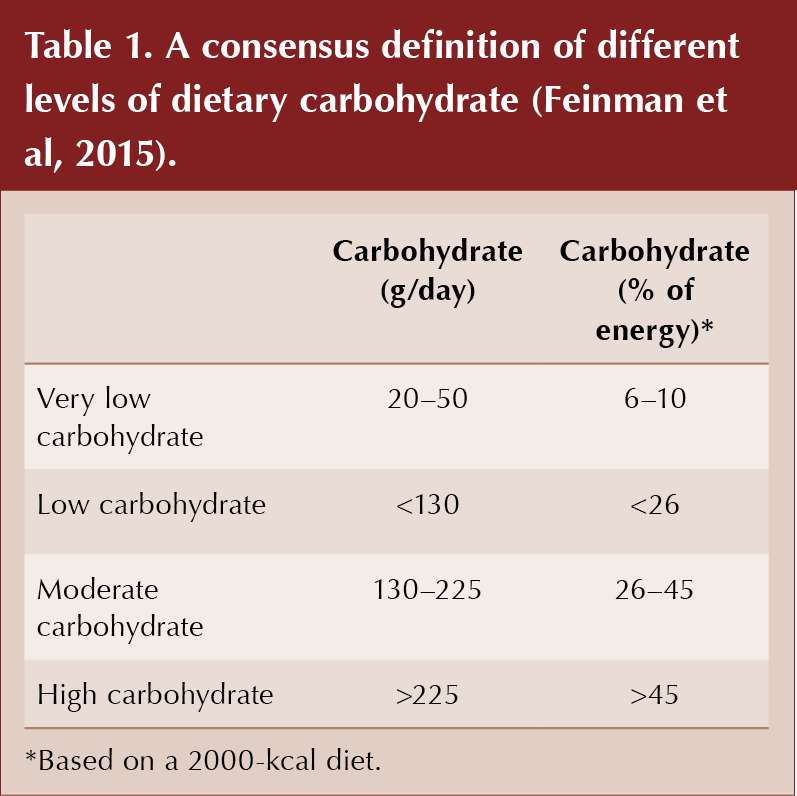
It is useful to clarify what actually defines low carbohydrate. Table 1 provides a consensus definition of different levels of dietary carbohydrate.
The percentage figures of total energy being supplied by carbohydrate are often quoted, but care must be taken. A study presented at the American College of Cardiology’s annual conference suggested that people on low-carbohydrate diets were 18% more likely to develop atrial fibrillation than people on a moderate-carbohydrate diet (Napoli, 2019). It defined low carb as <44.8% of daily calories!
Depending on an individual’s total energy intake, reporting carbohydrate as a percentage of it can tell a very different story – 45% of 800 calories is very different to 45% of 2300 calories. This is clear from the composition of the total meal replacement phase of DiRECT (the Diabetes Remission Clinical Trial).
DiRECT investigated whether it is possible to achieve type 2 diabetes remission with intensive lifestyle intervention within primary care. Of the 298 people recruited to take part in DiRECT, half received standard diabetes care from their GP, whilst the other half received a structured weight management programme (Lean et al, 2018). The programme included a low-calorie, nutrient-complete diet for 12–20 weeks followed by gradual food reintroduction and long-term support to maintain weight loss. Interestingly, the total-diet-replacement phase comprised a nutritionally complete, liquid-based diet providing 825–853 kcal/day – of which 59% was carbohydrate. As 1 g of carbohydrate provides 4 kcal of energy, simple calculations reveal that this provided 122–126 g of carbohydrate/day, which according to accepted definitions is a low-carbohydrate diet (Table 1). This illustrates that it is not simply about the proportion of carbohydrate consumed, but also the number of calories.
At 1 year, 68 (46%) of 149 intervention participants in DiRECT were in remission and 36 (24%) had achieved at least 15 kg of weight loss (Lean et al, 2018). The 2-year analysis assessing the durability of the intervention effect revealed that, at 24 months, more than a third (36%) of those in the intervention group were in remission and that this was closely linked to weight loss. Indeed, around two thirds (64%) of those who maintained weight loss of at least 10 kg were in remission after 2 years (Lean et al, 2019).
It is easy to calculate the macronutrient ratio in the total-diet-replacement phase of DiRECT, but very difficult to ascertain it once food begins to be reintroduced. Almost certainly, this varied between individuals. Maintaining the weight loss, by whatever means, seemed to be the key. That said, it would be unwise not to consider that carbohydrates raise blood glucose levels more than either fat or protein, particularly in a population in which there is a degree of glucose intolerance.
Reducing calorie intake (eating less) and increasing activity (moving more) may contribute to weight loss, but it rarely can be sustained. The DiRECT study employed a low-calorie diet – this does not represent a small reduction in total energy intake. When small changes to calorie intake are made, the body responds with hormonal adaptations to conserve energy and prevent starvation (which is why the “eat less move more” mantra has been widely criticised).
If we accept that people with diabetes are less able to handle excess carbohydrate than those without the condition, I find it illogical that the healthy eating advice to base all meals around starchy carbohydrates that is given to the general population is also given to those with diabetes. Surely some degree of carbohydrate restriction and increased carbohydrate awareness would be a more logical approach?
Jason Fung, a supporter of low-calorie, low-carb eating and intermittent fasting, uses an analogy that I have found useful when discussing eating patterns with my patients:
- Imagine that carbohydrate foods are converted to glucose that is used for energy, but if more is consumed than is needed it is stored in a fridge (the glycogen store in the body).
- When the fridge is full, any surplus glucose is stored in a freezer (where it is converted to fat for storage).
- If we never allow the fridge to empty (because we keep filling it with the glucose derived from eating carbs), then there is no need to use up what is in the freezer (i.e. body fat).
If there isn’t a store of glucose in the form of glycogen (as would typically occur on a low-carb diet), then the body will be forced to look for fat to break down for fuel.
Summary
The low-carbohydrate approach to weight management and improved management of type 2 diabetes has gained a great deal of attention in recent years from medical professionals and the public alike. We have seen a gradual shift in public health messages towards a reduction in carbohydrate intake as the scientific evidence has grown and provided encouragement. While long-term trials continue to assess how sustainable such dietary changes and health improvements are, many people are already looking at this approach as a source of hope and a way of regaining control of their weight and type 2 diabetes.
In the next issue of the Journal, I will discuss how health professionals in primary care can provide clear and safe guidance for patients interested in making such changes. Examples will be provided of resources that can be used to improve understanding of carbohydrates and how the body uses them, and I will summarise the key advice that I have given to help people lose weight and improve their diabetes control through diet.





Scotland-wide advice to inform the process of making injectable weight management drugs available and to prevent variation between Health Boards.
14 Nov 2024