Severe acute respiratory syndrome coronavirus 2 (COVID-19) caused the global pandemic that resulted in a national lockdown from 23 March 2020 (Dropkin, 2020). During lockdown, the way young people with type 1 diabetes (T1D) were monitored and supported changed from predominantly face-to-face consultations to remote contact. School and college closures along with restricted activity outside the home changed patients’ routines. Lockdown measures began to be eased from 10 May 2020. While the full national lockdown was 6 weeks in total duration, the majority of school children throughout the country did not attend school in May and June and outpatient services were still significantly restricted. The impact of lockdown on young people’s diabetes management was unknown, therefore glycaemic control (HbA1c and glucose levels) before and after lockdown was compared to assess the impact on this patient cohort.
Method
Data from individual glucose monitoring devices were collected across a 12-week period from 30 December 2019 to 22 March 2020 and compared to data captured between 30 March 2020 and 21 June 2020. HbA1c results from the same period before lockdown were compared to any HbA1c result taken after 23 June 2020 and before 13 August 2020. This avoided the inclusion of HbA1c results that reflected glycaemic control spanning both the pre- and post-lockdown period.
Patients were included in analysis if, in both the pre- and post-lockdown periods, data from ≥70% of total possible CGM or FGS readings or from >3.5 (>70%) SMBG readings per day were available. Patients conducting SMBG are advised to test their blood sugar at least five times a day as per national guidance (NICE, 2016),
Due to the alteration and temporary improvement in glycaemic control that can be experienced in the ‘honeymoon period’ soon after diagnosis (Abdul-Rasoul et al, 2006), patients with a diagnosis of T1D in the 12 months prior to 30 December 2019 were excluded from analysis. Patients diagnosed with T1D during the lockdown period were also excluded.
The mode of patient contact by paediatric diabetes specialist nurses (PDSNs) was logged in the electronic patient record. This information was accessed after the study period to determine the total number of face-to-face and telephone contacts before and after lockdown.
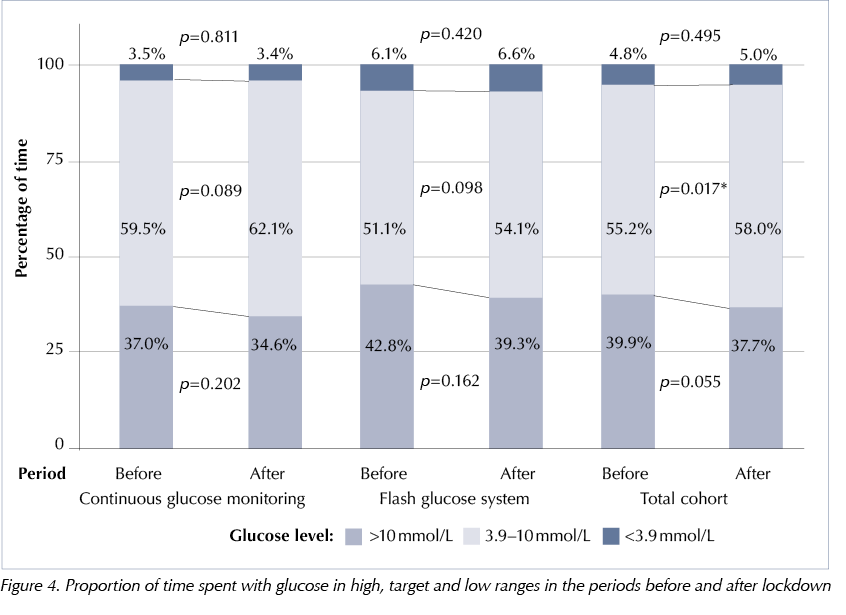
The primary outcome measures were HbA1c and mean glucose level. Secondary outcome measures were standard deviation in glucose levels and proportion of time spent within target range (for those using CGM or FGS). Target range was a glucose level of between 3.9 mmol/L and 10 mmol/L, as defined by international consensus (Danne et al, 2017). Glucose levels were recorded every 5 minutes by CGM and every 15 minutes by FGS. To accommodate short periods with missing glucose values, eg due to a sensor change or signal loss, time-in-range was considered continuous provided data points were ≤2 hours apart. For data >2 hours apart, the time frame was considered missing data and discounted.
Statistical analysis
Analysis was conducted using R (R Foundation for Statistical Computing, Vienna, Austria). The histograms and quantile–quantile plots of the data being compared were assessed and found to have normal distributions, which justified the use of parametric testing. Comparisons before and after lockdown were conducted using student’s paired t-test and comparisons between the three groups were conducted with analysis of variance (ANOVA). Comparison of categorical data exploring the method of patient contact was conducted using chi-squared test. The threshold for statistical significance was set at p<0.05.
Results
Demographics
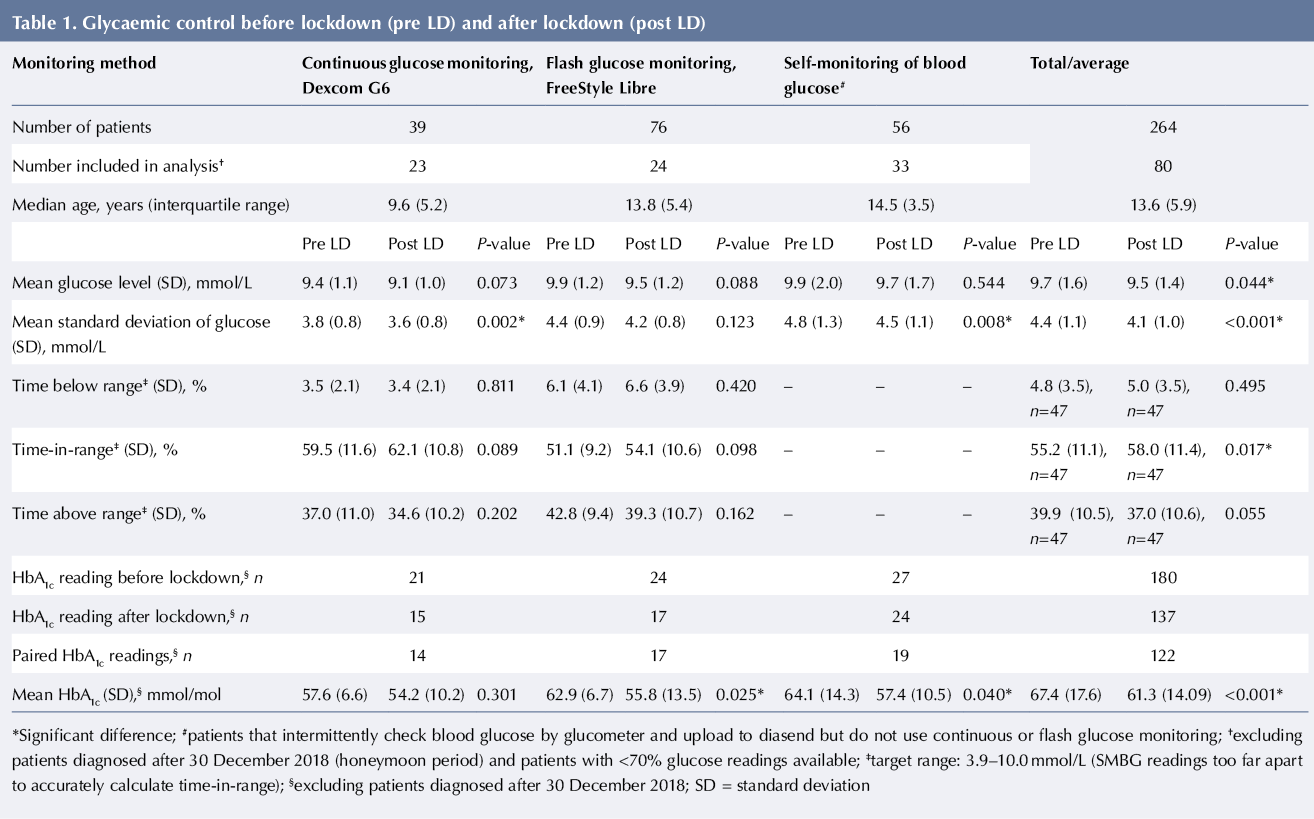
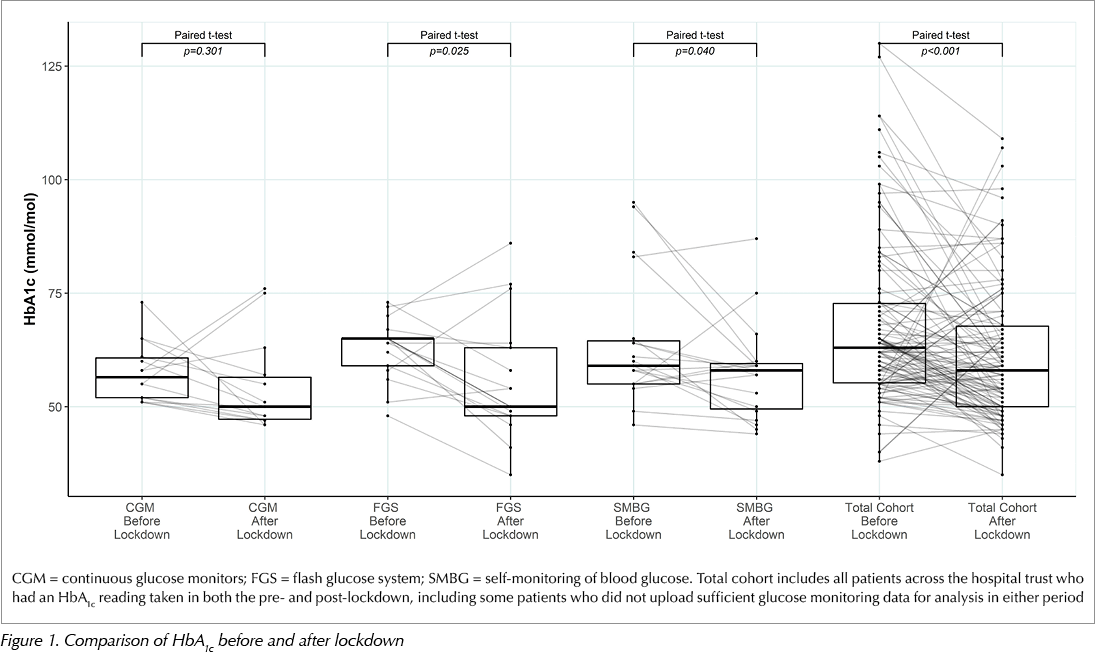
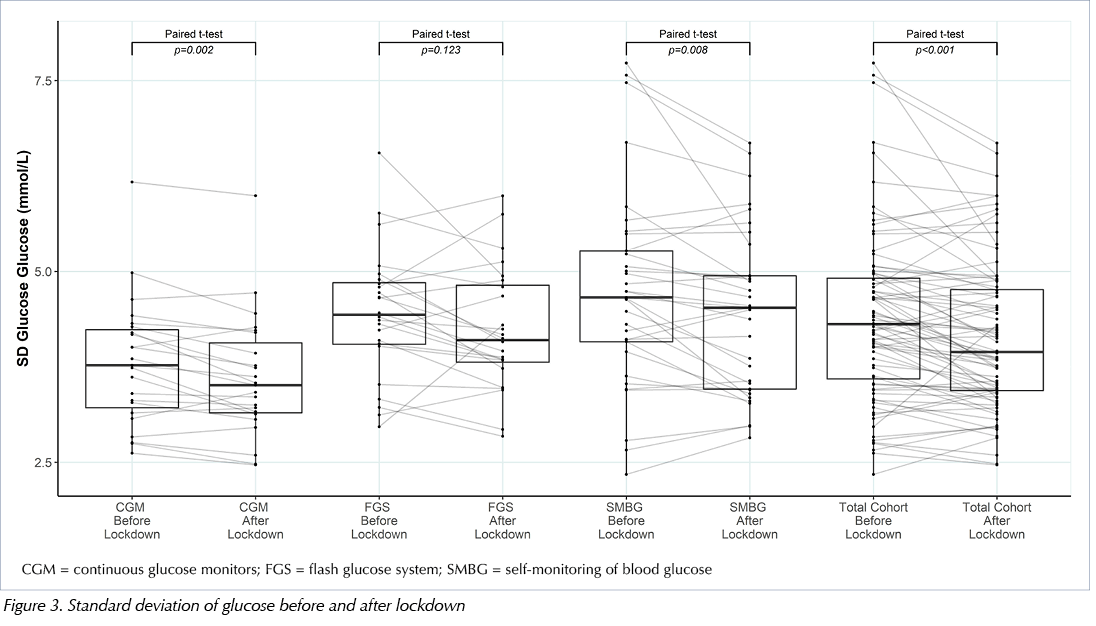
The records of total of 82 (42 male and 40 female) patients from Bassetlaw District General Hospital and 182 (93 male and 89 female) patients from Doncaster Royal Infirmary with T1D were reviewed. Forty-four were excluded as they had been diagnosed after 30 December 2018 and were therefore considered to be within their ‘honeymoon period’. Of the remaining patients, 122 had paired HbA1c readings taken in both pre- and post-lockdown periods. These patients had a median age of 14.2 years (interquartile range [IQR]=5.1). There were 47 patients beyond their honeymoon period using CGM or FGS and 33 using SMBG with sufficient data available for analysis, giving a total of 80 patients for full analysis (median age 13.6 years, IQR=5.9). Patient demographics and parameters of glycaemic control are given in Table 1.
The average age of patients in the CGM, FGS and SMBG groups differed significantly (p<0.001), making comparison between devices inappropriate. There was no between-group difference in time since T1D diagnosis (p>0.05). While in-depth information about intercurrent illnesses during this period was not available, none of the patients in the analysis required hospital admission during the study period.
Consultation format
The PDSNs recorded 245 face-to-face consultations before lockdown and 151 afterwards, representing a 39% decrease in the number of meetings held in person. There was a corresponding 30% increase in the number of telephone consultations, from 1751 before to 2269 after lockdown.
Glycaemic control
HbA1c levels significantly decreased from 67.4 mmol/mol (8.3%) to 61.3 mmol/mol (7.8%) across the total cohort (n=122), see Figure 1.
The reduction was significant in the 50 patients with adequate glucose monitoring data (60.9 mmol/mol [7.7%] versus 56.4 mmol/mol [7.3%], p=0.003). Significant HbA1c reductions in paired readings were recorded for the 17 patients using FGS (62.9 mmol/mol [7.9%] versus 55.8 mmol/mol [7.3%], p=0.025) and 19 patients using SMBG (64.1 mmol/mol [8.0%] versus 57.4 mmol/mol [7.4%], p=0.040), however the reduction in the 14 patients using CGM did not reach significance (57.6 mmol/mol [7.4%] versus 54.2 mmol/mol [7.1%], p>0.05).
Analysis of uploaded data from all 80 glucose monitoring devices revealed a lower mean glucose after lockdown (9.7 mmol/L versus 9.5 mmol/L, p=0.034), see Figure 2.
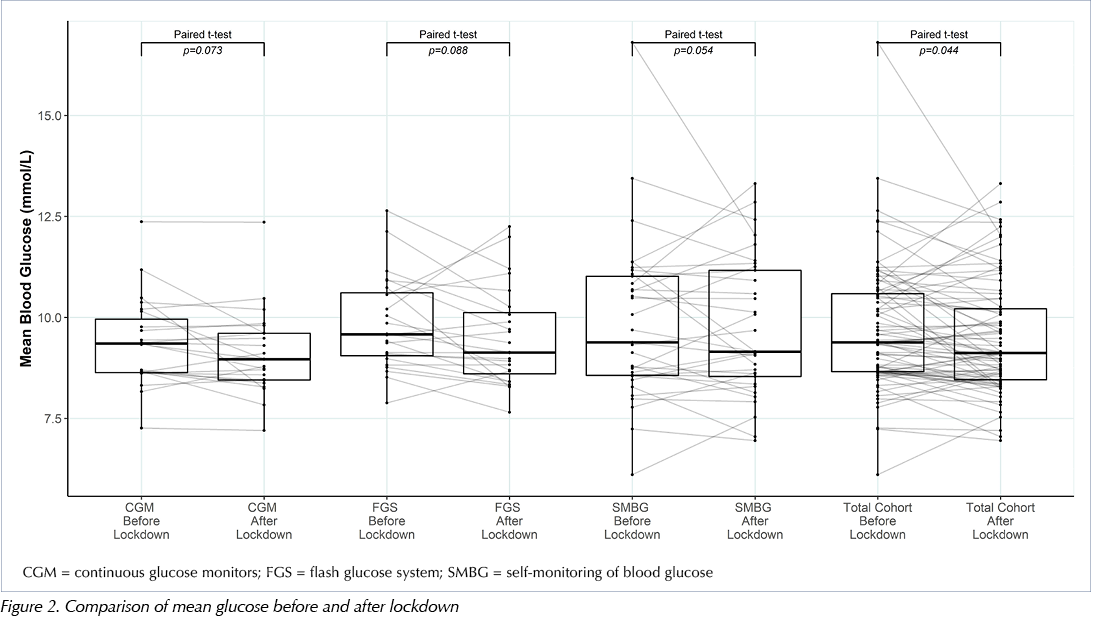
Glucose variability, as measured by the standard deviation of glucose readings, decreased significantly from 4.4 mmol/L to 4.1 mmol/L (p<0.001), see Figure 3.
Glucose time-in-range increased (p=0.017), with time above range decreasing at a level close to significance (p=0.055) and time below range remaining the same (p=0.495), see Figure 4. The mean and standard deviations for these comparisons are given in Table 1.
Discussion
This study shows an improvement in glycaemic control in children and adolescents with T1D after national lockdown and the closure of schools in the UK due to the COVID-19 global pandemic. HbA1c and mean glucose improved, with glucose monitoring data showing that this was a result of greater time spent within target glucose range, with no increase in time spent below range. The standard deviation of glucose levels decreased, showing less variability following lockdown.
After lockdown was announced, in line with UK national recommendations (Stevens, 2020), non-urgent face-to-face consultations within the hospital trust were cancelled. Consultant clinics were changed to virtual appointments after 23 March 2020, with few exceptions. In-person contact was gradually reintroduced in May, dependent upon the clinical need of individual patients, but at lower levels than prior to lockdown. During the lockdown, face-to-face contact by PDSNs – as logged in the electronic patient record – dropped by 39% but was replaced by a 30% increase in the number of telephone contacts. A ‘drive-by’ service was introduced during this period that complemented remote contact. This service enabled staff members to test patients’ HbA1c or upload glucose monitoring data if the patients and their families did not have the ability to do so themselves. The diabetes team experienced very good engagement with remote contacts, likely aided by the restrictions placed on travel and activities throughout the country that resulted in families being easier to contact. PDSNs aimed to contact patients at least fortnightly, although there was flexibility in targeting patients with the greatest clinical need. Reduced staff travel time meant team members were able to provide broader patient support. It was observed that patients who previously were averse to uploading glucose data become more proactive in doing so during lockdown.
During the 2020 lockdown period glycaemic control improved in adults with T1D using CGM in Scotland, Italy and Spain (Bonora et al, 2020; Capaldo et al, 2020; Dover et al, 2020). However, a group in India who surveyed patients with T1D who were performing SMBG during lockdown found increases in average blood glucose and HbA1c, which was attributed to the reduced availability of blood glucose test strips (Verma et al, 2020). A study of 34 children in Greece showed similar glycaemic control in patients on insulin pump therapy before and after lockdown, but a significant change in their meal schedules (Christoforidis et al, 2020). To the best of the authors’ knowledge, the current study is the first to analyse the impact of lockdown on glycaemic control in children and adolescents with T1D in the UK.
Regular televised UK government updates and a strong focus in the media have resulted in greater health awareness during the pandemic (BBC, 2020). The increased risk of mortality in those with diabetes who contract COVID-19 may have crystallised the importance of glycaemic control within families (Huang et al, 2020). While circumstances will have differed across the families in the cohort, it is likely that most patients had more time to concentrate on diabetes care as a result of reduced school and extracurricular activities as well as an increased level of supervision from parents. While PDSNs have used telephone contact with patients consistently for many years, families have appreciated the convenience of being able to liaise with physicians and dietitians in the diabetes team over the telephone rather than having to attend face-to-face appointments, which may have contributed to improved glycaemic control.
The strengths of this study are the large patient cohort included and the significant amount of reliable data available from modern glucose monitoring systems. While CGM and FGS measure interstitial glucose, the sensor models used by patients at Doncaster and Bassetlaw Teaching Hospitals have been shown to correlate very closely with blood glucose, are factory calibrated and show a low mean absolute relative difference in independent testing (Welsh et al, 2019). The glucometers used by patients performing SMBG are linked directly to diasend software, removing the possibility of human error or bias when recording or transcribing results.
This was a retrospective review of real-world local data and care should be taken before applying the findings to other patient populations. The cohort was heterogenous, as school closure was not universal and not all families stayed at home throughout this period; workers deemed essential to the functioning of society remained in work and were able to send their children to school. There are no data on the proportion of people in this study who stayed at home or to what degree they complied with government advice during lockdown. While no patients required hospital admission during this period, data on episodes of mild illness are lacking. The national lockdown was designed to reduce the spread of COVID-19 infection, but also likely reduced the spread of other infectious diseases that may have contributed to the observed improvement in glycaemic control.
Good glycaemic control in children and adolescents improves short-, medium- and long-term health outcomes (Prince et al, 2007, Monaghan et al, 2015). Modern technology affords the luxury of maintaining good patient contact and monitoring blood sugar levels without the inconvenience of families having to travel to attend appointments. The data highlight that T1D is challenging to manage outside the home. Continued contact with patients and families in ways convenient for them is recommended to maintain engagement, as is focusing education on how to manage T1D around changes in routine, particularly school and physical exercise. This study reiterates the importance of good communication between members of the diabetes team, carers of those with T1D and school staff to achieve good glycaemic control.
Conclusion
Glycaemic control in children and adolescents with T1D improved in the 12 weeks following national lockdown during the COVID-19 pandemic. This finding demonstrates the difficulties associated with managing T1D around school pressures, meals away from home, social engagements and peer pressure. It also highlights the importance of patient and carer education about managing T1D outside the home. Increased remote contact with patients with T1D has not been detrimental to glycaemic control.





NHSEI National Clinical Lead for Diabetes in Children and Young People, Fulya Mehta, outlines the areas of focus for improving paediatric diabetes care.
16 Nov 2022