An important area of investigation for the NHS in the UK, and in healthcare worldwide, is to determine both how much time nurses expend and the level of nursing expertise necessary to deliver care to different patient groups in a variety of environments. It is challenging to do this with accuracy as nursing, in common with many other human activities, is constantly changing and has a high level of complexity (Hall, 1964; Pitkäaho et al, 2014; Diabetes UK, 2016). Even determining the relevant information that needs to be collected to produce a model may be challenging (Ebright et al, 2003) and there is no current consensus on this issue.
Current estimates from 2017 to 2018 put the number of people with diabetes in the UK at 3 809 119 (Diabetes UK, 2018). The prevalence of diabetes is rising, and with it increases in demand for diabetes services without increasing diabetes specialist nurse (DSN) numbers. This has raised concerns from the DSN workforce that its workload is impacting on patient care and safety (Diabetes UK, 2016).
Specialist nursing work varies in the UK. The level of practice and job title, for example, are not a reliable proxy for complexity of practice (Leary et al, 2016). Nurse specialists in the UK tend to work at a number of levels of complexity, provide a varying range of interventions and carry out their work in different service arrangements depending on location. All of these factors can affect workload burden. Other relevant issues include complexity of patient needs (Kentischer et al, 2018) and access to other members of the multidisciplinary team (MDT; Punshon et al, 2017).
In order to model a future UK diabetes nursing workforce, demand modelling is needed to understand the need for diabetes nursing interventions. This includes understanding how the current workforce meets demand, what work is left undone, how much overtime (paid and unpaid) is required to meet demand and the available skill mix in terms of complexity.
Study aim
The aim of this study was to understand the work and distribution of workload of DSNs in various healthcare settings.
Methods and data collection
Studies of other nursing specialties have identified a number of common factors that typically influence specialist nurse workload. Examples include relationships with other members of the MDT (Punshon et al, 2017), complexity of caseload (Leary and Anionwu, 2014; Leary et al, 2018), access to administrative assistance (Quinn, 2011), access to other services (National Cancer Action Team, 2013), and education and experience (Oliver and Leary, 2010). Issues such as access to non-medical prescribing (Courtney et al, 2012) and the ability to independently request investigations are also significant factors. Where nurse specialists are able to prescribe and independently request investigations, this enables and empowers them to make independent decisions rather than “door hang” for the decisions of others.
An understanding of these factors informed the construction of a 22-item questionnaire exploring demographic data, caseload and workload for diabetes nursing specialists, using consensus from clinical, patient and academic experts based on a previously employed national study (Leary et al, 2018). The questionnaire was designed to gather data on activity and complexity of the specialist nursing services provided, and used a format similar to the national optimum caseload modelling project (National Cancer Action Team, 2013). This was transferred to an online survey tool, administered using a SurveyMonkey secure account. The survey link was distributed through the DSN Forum Facebook group between February and April 2019. In total, 243 participants responded to the questionnaire. A single response could only be submitted from each computer. Analysis of the survey took place in May 2019.
Data analysis
Data were exported into Microsoft Excel and analysed using descriptive statistics; for example, demographics, workload, educational background, pay band and length of service. Free-text comments were analysed using NVivo 11 (QSR International, Melbourne, Australia) and thematic content analysis (Anderson, 1997). Thematic content analysis is the approach best suited to analysing free-text questions in an otherwise quantitative questionnaire, as it does not rely on interpretation of data but instead reflects a “low hovering over the data” (Anderson, 1997).
Ethical approval
This study was considered to be a service evaluation, and the local regional Ethics Committee deemed that ethical approval was not required for this study. This was confirmed using the Health Research Authority decision tool.
Results
Response rate
Responses to the SurveyMonkey workload questionnaire were received from 243 nurses who fully or partially completed the questionnaire. The DSN Forum has 1385 members (November 2019 data); however, not all of the members are nurses, so it was not possible to calculate a response rate.
Respondents’ demographic data and epidemiology of diabetes in the UK
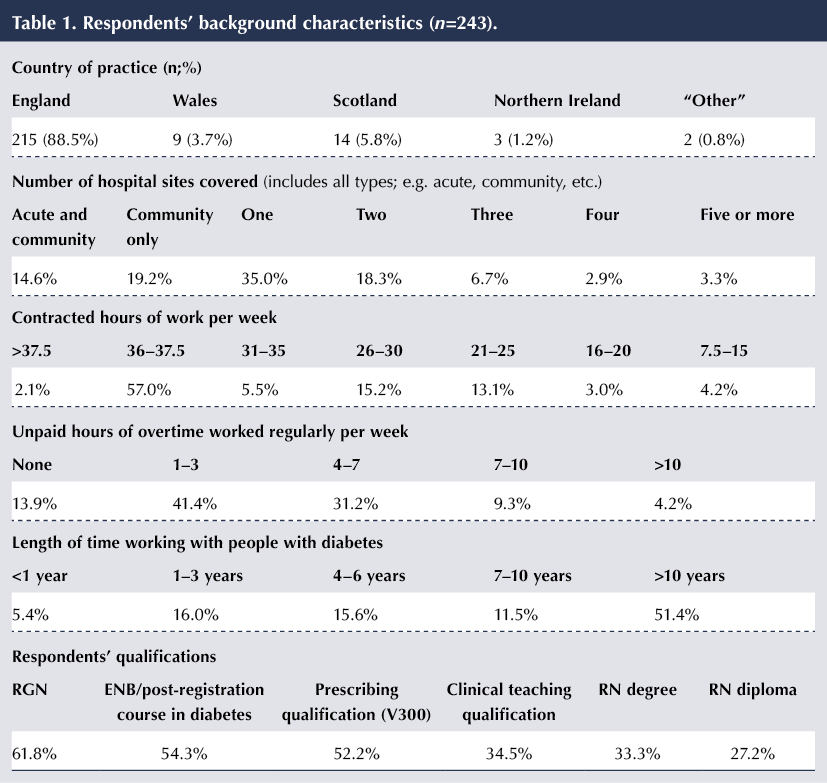
The country of practice, number of hospital sites covered, number of hours worked per week, unpaid overtime worked per week (including working through meal breaks), type of practice, length of time working with people with diabetes and educational qualifications are summarised in Table 1.
Respondents’ unpaid overtime worked
No unpaid overtime was reported by 13.9% (33/237) of respondents; 41.4% (98/237) reported between one and three hours per week; 31.2% (74/237) reported four to seven hours; 9.3% (22/237) reported seven to ten hours; and 4.2% (10/237) reported more than ten hours per week (Table 1).
In total, using median hours for each category, this equates to 923 hours of unpaid overtime per week for the group as a whole. These 923 hours represent 24.6 whole-time-equivalent posts, or £17 546 of unpaid work per week contributed by the group (assuming a mid-spine-point Band 7 rate of £19.01 per hour).
Respondents’ job titles
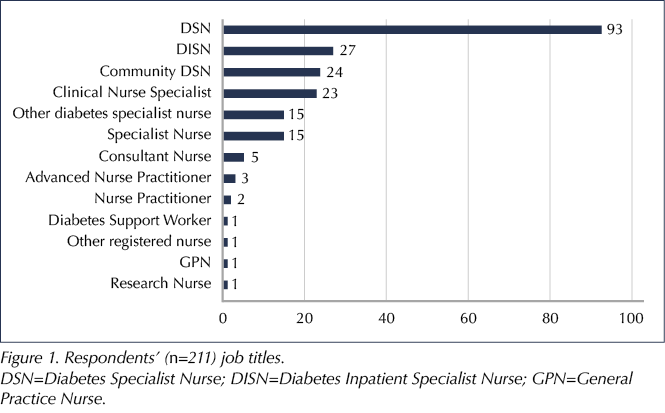
Diabetes Specialist Nurse was the most common job title, in 44.1% (93/211) of respondents. Diabetes Inpatient Specialist Nurse (12.8%; 27/211), Community Diabetes Specialist Nurse (11.4%; 24/211) and Clinical Nurse Specialist (10.9%; 23/211) accounted for a further 35.1% of respondents’ titles (Figure 1).
In the free-text comments, a number of different job titles were reported: Paediatric DSN (n=11), Diabetes Matron (n=2), Lead Nurse Diabetes (n=3), Advanced Specialist Practitioner Diabetes (n=2), Inpatient DSN (n=2), and Diabetes Surgical Specialist Nurse, Diabetes Nurse, Diabetes Service Lead, Honorary Clinical Professor, Diabetes Specialist Foot Care Nurse, ThinkGlucose Project Lead, Lead DSN, Specialist Diabetes Midwife, Lead Nurse for Diabetes and Endocrinology, Community Diabetes Specialist Practitioner, Paediatric Diabetes Clinical Nurse Specialist, Diabetes Care Facilitator, Locality DSN, Practice Nurse, Genetic Diabetes Nurse and Associate Diabetes Specialist Nurse (n=1 for all).
Administrative support provided to respondents
Respondents were asked how much administrative support (help with typing letters or doing routine non-clinical administration) they received each week. No administrative support at all was reported by 42.2% (100/237) of respondents; 19% (45/237) had support only for clinical letters; 13.9% (33/237) had 1–5 hours’ support; 4.6% (11/237) had 6–12 hours’ support; 5.9% (14/237) had 13–20 hours’ support; and 14.4% (34/237) had more than 20 hours’ support per week.
Unfilled and frozen vacancies
To ascertain the level of unfilled and frozen posts, respondents were asked how many, if any, posts were unfilled in their speciality. Two respondents reported frozen posts, while 50% of respondents (101/202) reported at least some unfilled DSN posts in their team.
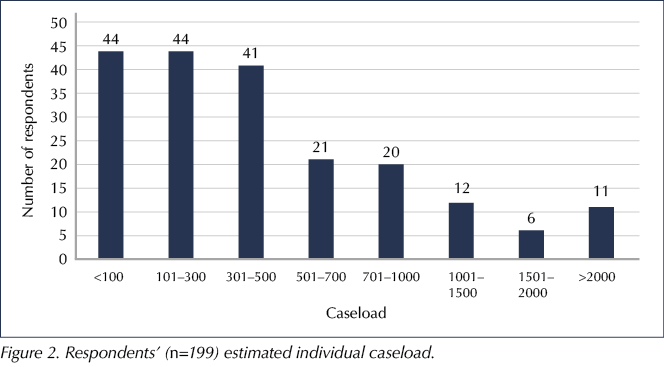
Respondents’ estimated caseload
Respondents were asked to estimate their individual caseload. There was a wide range of caseloads reported, with <100–500 being the most common (64.8%; 129/199 respondents). Caseloads as high as >2000 were reported (Figure 2). Using the median number for each category, this gives a total caseload of 101 750 patients for the whole group.
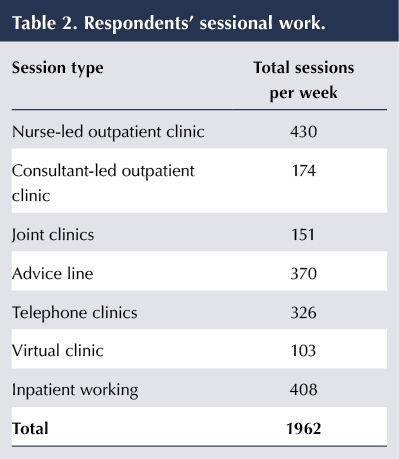
Respondents’ sessional work
A total of 1962 sessions per week were recorded by the respondents. Inpatient working took up 408 sessions. Clinics took up 1184 and advice lines 370 sessions (Table 2).
Analysis of free-text comments
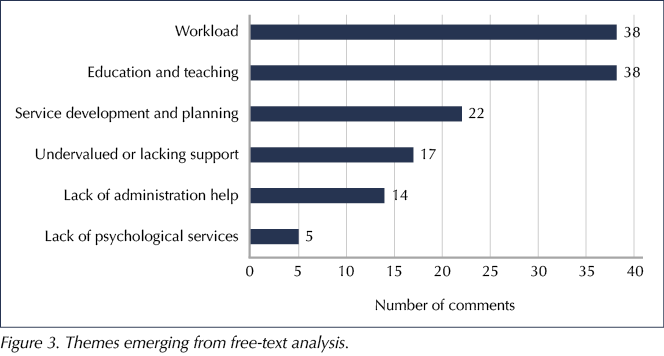
A number of themes emerged from analysis of the free-text comments made by respondents. These fell into a number of categories, summarised in Figure 3.
Theme 1: Education and teaching
Thirty-eight comments involved issues with education and teaching. These were focused on both staff and patient education and training. A lack of time for education was the biggest issue, and some respondents felt the survey did not cover education in sufficient depth. Typical comments included:
• “Do not have sufficient time for staff education which would save clinical work time.”
• “Unable to give patients the time and in-depth education that they deserve and need.”
• “No time as part of contracted hours to develop patient education.”
• “I can’t seem to ever make time for my admin or training. All my time is spent with my patients and there is nothing left over.”
• “The survey has missed out a large proportion of work I do including Diabetes Structured Education, healthcare professional education and working alongside community/primary care colleagues assessing competency and upskilling.”
Theme 2: Workload
Thirty-eight comments referenced workload, lack of adequate staffing or variations on not having enough time to complete their work. Typical comments included:
• “Missed meal breaks and high stress levels.”
• “We need more staff for the hugely increased numbers of patients. We are just back up to full numbers of DSNs – after a long period of very low staffing due to people leaving, long-term sickness, people not replaced, etc. We actually have the same (or maybe slightly less) number of DSNs now that we did when I started in 2001. In 2001 there were 6000 [patients] on the register in our town. Now it’s about 20 000. I fully expect 7-day working to be mentioned again soon – we did a trial a couple of years ago but staffing levels were abominable and it was abandoned.”
• “No time to do anything other than enough to keep patient safe. Would like to be able to work with patients to make best use of their pumps/CGM, etc., but never time to do more routine work – as urgent work takes up time.”
• “We are short staffed and firefighting most of the time.”
• “Most things get done due to working extra hours. These are not paid for!”
• “Workload just keeps on increasing together with more responsibility. However the pay remains static.”
Theme 3: Service development and planning
Twenty-two comments referenced issues with service development, audit and planning. Typical comments included:
• “Not much time for planning and preparation.”
• “Ideas for service development to implementation is longer than required, this is at times due to motivational force; i.e., if the right persons are interested, initiative moves forward; if not, halted and can take years if you do not give up before.”
• “I don’t always feel I have enough time to develop our service, which could improve service provision. It would be great if we could go to our managers and state recommendations on the number of outpatient DSNs to caseload. There is that for inpatient DSNs, we need one for outpatient DSNs.”
• “Audit always comes second as a priority, which is shameful as we are supposed to be delivering evidence-based practice.”
Theme 4: Feeling undervalued or lacking support
Seventeen respondents reported either feeling undervalued or lacking in support or empowerment for their work. Typical responses included:
• “Lack of empowerment. Very hierarchical.”
• “Feeling undervalued and unsupported by Manager.”
• “Diabetes not seen by our Trust as an essential service, staff grossly undermined by exec. team as they have no understanding of our role.”
• “I’m a senior Band 7 with MSc and prescribing. More and more I’m taking complex cases previously managed by medical staff. Whilst I have the skills to do so, I don’t get the support from managers or the recognition for what I do. Specialist nurses are the glue holding the NHS together but no-one cares about us.”
• “CNS posts are always being reviewed, currently filling out another one after only just doing one less than 6 months ago in a different format.”
• “The challenges are that it is always the nurses that pick up the pieces of whatever someone else can’t/won’t do, from admin staff, play staff to dieticians!”
Theme 5: Lack of administrative help
A lack of administrative assistance or time to complete administration was reported by 14 respondents. Typical comments included:
• “As lead inpatient nurse I have very limited time to complete admin tasks – e.g. off-duty appraisals, attend meetings – it is always fitted in around other things. Very stressful and has increased in the last 1–2 years.”
• “We get no admin time so updating policies, etc., has to be done in own time.”
• “Desperately need admin support.”
• “In the administration support section there was not an answer that was totally applicable to me. I do have admin support for booking of patient appointments into clinic but I write all my own clinical letters that go back to GP. I do feel that all the documentation I am expected to do takes a up a lot of my time and it is catching up on these, referrals, chasing blood results, etc., that I end up doing outside of my working hours.”
• “No admin – had money for a Band 3 but been taken away from us.”
• “Administrative time is precious!”
Theme 6: Lack of psychological services
Finally, the lack of psychological services and social issues was raised by five respondents. These comments were:
• “We currently don’t have access to any psychological services/support for our patients with type 1 diabetes and I feel that this is letting our patients down and there is a huge need for it, particularly in our area.”
• “Social problems… housing problems… psychological problems are all issues that patients have but we often cannot offer constructive help. I am particularly keen to try and get a clinical psychologist to work with us but this has been a very long-standing issue i.e. lack of funds to achieve this for our patients. This concerns me as many patients have depression, self-neglect problems, etc.”
• “We have no psychology support.”
• “Social problems. Child protection. All supported by social worker and family support worker.”
• “Very difficult trying to work with demand of the job and psychological support for patients struggling with mental health issues.”
Discussion
Specialist disease-specific nurses are known to enhance the quality of care and patient experience (Health Service Journal, 2015) and can be productive not only in terms of quality but also in terms of efficiency, such as the avoidance of unnecessary admission to an acute inpatient unit (Quinn, 2011; Baxter and Leary, 2014).
Caseloads as high as 2000+ patients were reported in this study. There are a number of potential reasons for these high caseloads. One potential issue is unfilled DSN posts, with 50% of respondents reporting at least some unfilled posts in their team. This figure is substantially higher than that from a 2016 survey, which found that around one third of respondents had vacancies in their team (Diabetes UK, 2016), and a 2013 survey of 71 DSNs which reported that only 18% had DSN vacancies in their Trust (Diabetes UK, 2014). Another factor apparent from this study is the amount of unpaid overtime currently being carried out by DSNs. Only 13.9% of respondents regularly worked no unpaid overtime. The amount of unpaid overtime carried out by the remaining respondents equalled an estimated 24.6 whole time equivalents. Diabetes UK (2016) found that almost 90% of DSNs reported working above their contracted hours, with 25% working in excess of 5 hours’ overtime each week. Additionally, evidence suggests that DSNs have limited access to professional development and opportunity for study leave and research, due to restraints in capacity (James et al, 2009).
It is clear from the workload analysis that there is much variability in and different levels of service provision. The group recorded 1962 sessions that were taken up with programmed clinical activity. The majority of this time was taken up by clinics (1184 sessions) and advice lines (370 sessions).
The analysis of the free-text comments confirmed much of the above, with issues such as access to education, workload, lack of time for service development and planning, lack of administrative assistance and lack of access to psychological services all being raised. These issues have also been highlighted recently in other specialist nursing groups, such as district nurses (Queen’s Nursing Institute, 2019).
It is also apparent that, because of the variability of service provision, local circumstances should be taken into account, such as the availability of administrative help, which remains a burden for some DSNs. In other specialisms, provision of administrative and support workers has increased productivity; for example, administrative workers allowed multiple sclerosis specialist nurses to proactively manage their caseload, resulting in reduced emergency admissions (Leary et al, 2015). Another local factor that can influence caseload is the complexity of patients.
Just under half of respondents (47.8%) were not independent prescribers, which leads to so-called door hanging: having to access other professionals to sign off decisions or recommendations. Previous work has shown that it is generally more efficient if case-managing advanced practice nurses can sign off their own prescriptions and investigations. Diabetes nurse prescribers have been found to reduce patient length of stay on average by three days (Carey et al, 2008). A comparison of prescribing and non-prescribing diabetes nurses in general practice found significantly higher levels of satisfaction among prescribing nurses’ patients (Courtenay et al, 2015).
Study limitations
Limitations to this study include obtaining data via an online survey from a self-selecting group. The study was a retrospective, “one-point-in-time” study and relates only to the situation encountered by respondents in the UK.
Conclusion
The findings of this study will help to understand the workload and productivity of the DSN workforce in the UK and demonstrate areas that need attention. These data could be used to inform workforce modelling in the future.
Funding
This work was part of a larger modelling study funded by the South West London Health and Care Partnership and North Central London (Royal Free) NHS Trust.
Acknowledgements
The authors would like to thank Amanda Epps of the DSN Forum for distribution of the survey, and all those who took part in data collection.





NHS type 2 diabetes prevention initiative reaches more people than ever.
5 Jun 2025