In the lifetime of many people with diabetes, the long-term outlook has been transformed by evidence-based medicine; for example, tight glycaemic control increasing life expectancy, as shown by the DCCT and UKPDS studies in people with type 1 and type 2 diabetes, respectively (Nathan et al, 1993; UK Prospective Diabetes Study Group, 1998). However, these studies also showed that the tighter the control the higher the risk of hypoglycaemia.
It is clear that the older population with diabetes has special needs and concerns relating to hypoglycaemia (Kirkman et al, 2012; Grajower, 2018), and there has been a review of safety for this cohort, with new glycaemic targets set (Laubscher et al, 2012; American Diabetes Association, 2019). Hypoglycaemia has greater consequences for older people with diabetes, as they are more prone to falls and fractures (Nicodemus et al, 2001; Montero-Odasso and Speechley, 2018). They also have an increased risk of mortality following hospital admission for hypoglycaemia, and some may also experience permanent neurological damage (Sinclair, 2006).
With more people with diabetes living longer, Sussex Community NHS Foundation Trust (SCFT) is seeing an increasing workload for community nurses to support people with their insulin management. Within the Trust there has been a growing number of elderly, often frail, single people needing community support to manage their day-to-day diabetes needs.
Background
SCFT is the main provider of NHS community health and care services across West Sussex, Brighton and Hove, and the High Weald Lewes Havens area of East Sussex. It provides a wide range of medical, nursing and therapeutic care to over 8000 people a day, working to help people plan, manage and adapt to changes in their health, to prevent avoidable admission to hospital and to minimise hospital stay. Both locally and nationally, there has been an increase in the number of people needing to have their insulin administered by the community teams, and SCFT has recognised the increasing workload and potential risk to patients and their ability to administer some insulin regimens at the optimal time(s).
Insulin regimens for these individuals tend to be either a once-daily basal insulin or a twice-daily biphasic insulin, which needs to be administered with the morning and evening meals. Staffing for the community nursing team has been a challenge; the team’s core hours are 8 am till 6 pm, and there is a high demand for insulin administration around the start and finish of these core hours. SCFT community staff estimated the cost of a nurse visit (Band 3–6 community nurse) at £40. The Personal Social Services Research Unit (2017) puts costs between £24 and £44 per visit.
Capillary glucose levels are generally only checked when the community nurses visit to administer insulin. This gives only a snapshot of control and often takes place after meals, making it difficult to safely titrate insulin doses. However, with the development of an affordable, factory-calibrated glucose monitoring system, the FreeStyle Libre flash glucose monitor, we are now able to review glucose levels in a systematic way for our frail elderly patients who need district nurses to administer insulin. In studies, continuous glucose monitoring has revealed hypoglycaemia risk in elderly patients on insulin (Ishikawa et al, 2018); however, such monitors need calibration, which increases the workload for the community nursing teams.
Project
The community diabetes specialist nurse (DSN) team undertook a virtual review of all its patients who have insulin administered by the community nursing team, in order to identify whether those who were on pre-mixed biphasic insulin regimens were being subjected to unnecessary risk of hypoglycaemia, as the timings of these injections and the patients’ main meal times varied.
The participants within this case series had the following characteristics:
- Type 2 diabetes.
- Insulin administered by the community nursing team.
- Stable blood glucose levels (above 4 mmol/L and under 10 mmol/L) when the community nurses checked during their visits.
- Patients or carers able and willing to scan a flash glucose monitor to collect data for analysis.
This project had support from Abbott, who provided the team with a supply of FreeStyle Libre glucose sensors and readers. A Libre sensor was fitted by the DSN and education given to the carers and patients regarding the use of the device. Going forward, this device can be fitted by the community nursing staff following training, and the data can be uploaded via resources such as Diasend and LibreView, to be reviewed by the DSN.
After application of the device, the participants’ glucose levels over the first two days were reviewed by the DSN. Following this, any changes to medication were agreed with the participants after discussion of the risks and benefits. The decision was made to use the ultra-long-acting insulin degludec (Tresiba) as this has a lower incidence of hypoglycaemia compared with other analogue insulins available in a 100-units/mL preparation (Rodbard et al, 2014), and because the flexibility of its timings for injections (Meneghini et al, 2013) would enable the community nursing teams to manage their workload in a more effective way, in line with local clinical practice and the drug’s Summary of Product Characteristics.
The participants’ total daily dose of basal insulin was calculated by adding together their current daily prescribed insulin doses with the prandial portion of the biphasic mixed insulin regimen removed (for example, in the case of Humulin M3, 30% of the total daily dose is prandial insulin; therefore, a 30% reduction was made to the dose). A further 20% reduction in dose, to reduce the risk of hypoglycaemia (Hope et al, 2018), was made to calculate the initial starting dose of once-daily Tresiba.
The flash monitoring data were reviewed for a second time at the end of the first week of the Tresiba regimen, and further adjustment of the insulin dose was made as needed.
Results
Four participants are presented in this case series. It was clear from the first two days of flash monitoring data that the participants’ blood glucose levels were not stable, and they were having hypoglycaemia at times when they were alone and often overnight.
Participant 1
This 91-year-old individual has type 2 diabetes complicated by heart failure, and has been on insulin since 2004. At the start of the study, he was receiving Humulin M3, 20 units in the morning and 22 units in the evening (total daily dose, 42 units). The community nurses were visiting him at around 8 am and then between 4.30 and 5 pm.
His flash data for the first two days on this regimen can be seen in Figure 1. It is clear that this frail, 91-year-old patient was having hypoglycaemic episodes overnight, and his glucose levels were far too low for his safety.
In response to the flash data, the total daily dose was reduced by 30% to account for the prandial insulin and then by a further 20% to account for the hypoglycaemia. This gave a starting dose of 24 units of Tresiba.
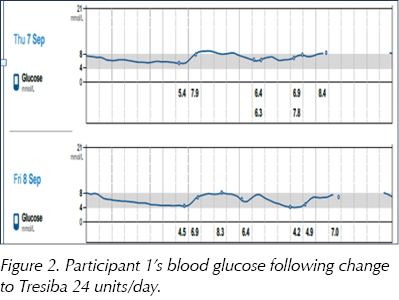
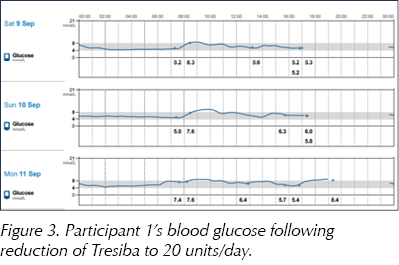
The subsequent scan (Figure 2) revealed that this dose of 24 units had not sufficiently reduced his risk of overnight hypoglycaemia, so the dose was reduced by a further 20% to 20 units/day. Figure 3 shows the scan results following this reduction, and it was agreed to reduce the insulin dose further to 18 units/day to maintain safety.
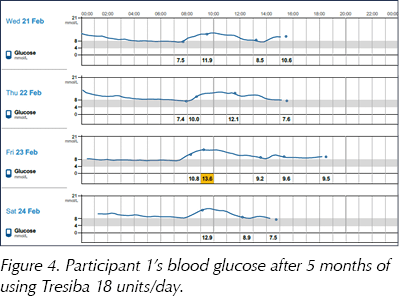
This medication change has reduced the number of community nursing visits by 365 per year. With a cost per visit of £40, SCFT estimates that this has reduced annual costs by £14 600. Another sensor was applied 5 months later, and the participant has remained stable on once-daily Tresiba 18 units/day (Figure 4).
Participant 2
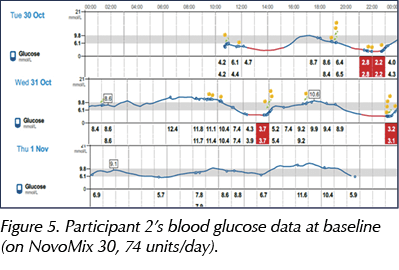
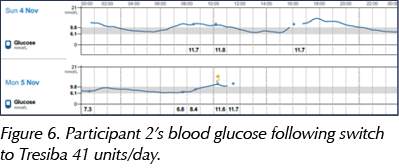
This 63-year-old lady has had type 2 diabetes since before 2009 and was started on insulin in June 2015 following the failure of all oral agents and a rising HbA1c. The community nurses have been needed to administer her insulin from the start. This lady is often not available for an appropriately timed afternoon injection. At the start of the study she was on NovoMix 30, at a dose of 31 units in the morning and 43 units in the afternoon (total daily dose, 74 units). Again, the flash data showed frequent hypoglycaemia (Figure 5), and so the daily dose was adjusted to account for both the prandial insulin and hypoglycaemia.
Following the switch to Tresiba 41 units once daily, the incidence of hypoglycaemia was reduced (Figure 6). The removal of the afternoon insulin injection has also improved the participant’s quality of life and gave her more freedom with her day, whilst maintaining safety.
Participant 3
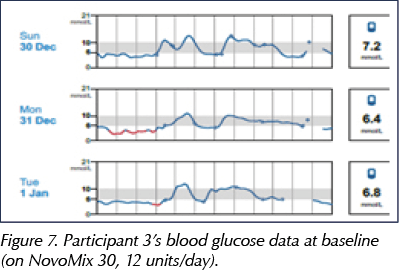
This 85-year-old lady has had type 2 diabetes since 1997 and has been on insulin since November 2011. Although at present she is independent in the management of her insulin, her HbA1c was 47 mmol/mol (6.4%) and she is under the care of SCFT for heart failure. She was taking NovoMix 30 at a dose of 6 units in the morning and 6 units in the evening (Figure 7). The stopping of her insulin was managed over the 2 weeks of wearing the sensor, and she was visited daily by the DSN in the 24 hours before and after stopping insulin. The insulin doses were first reduced by 50% and then the decision was made to stop the insulin altogether, resulting in reduced hypoglycaemia (Figure 8).
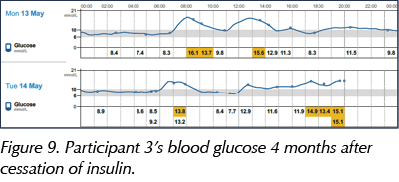
At 4 months after the intervention, the participant’s blood glucose levels have remained stable (Figure 9).
Participant 4
This participant is a 73-year-old gentleman who has had type 2 diabetes since 1991 and has been on insulin since 2004. He had recently had an admission to hospital for hypoglycaemia and had his Novomix 30 reduced to 16 units in the morning and 10 units in the evening. He was having his insulin managed by the community nursing team. This gentleman was being cared for in a nursing home at this time and was unable to express symptoms of hypoglycaemia due to his progressive dementia (Figure 10).
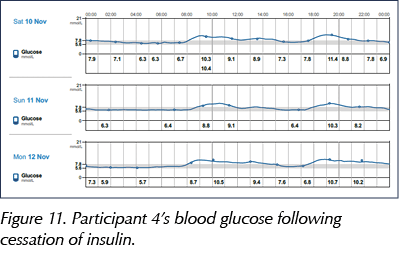
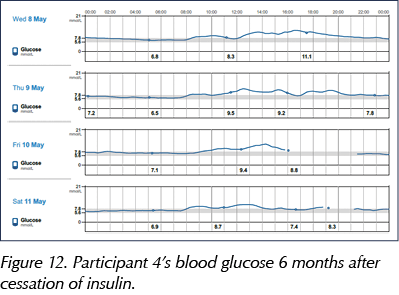
His insulin was stopped, reducing his hypoglycaemia (Figure 11). Since then, his HbA1c has increased from 49 to 72 mmol/mol (6.6% to 8.7%), prompting an enquiry from the GP as to the need to add in medication to manage this. As a result, a new sensor was attached to review his glucose levels 6 months after stopping the insulin, and showed that he remains safely managed without the insulin (Figure 12).
Cost savings
The reduction of visits within these participants equated to 1460 fewer community nurse visits in one year, delivering a cost saving of £58 400 in nursing visits alone, in addition to the use of 1460 fewer needles and test strips, and more stable diabetes.
Discussion
With an understanding that it is difficult for community nurses to achieve consistent delivery of insulin at exact times, the use of insulin degludec in two patients enabled the community nurses to be more flexible with the timings of the insulin administration without increasing the patient’s risk of hyper- and hypoglycaemia. The use of degludec has been shown to reduce hypoglycaemia and particularly nocturnal hypoglycaemia (Ratner et al, 2013).
Studies have shown both increased frequency of hypoglycaemia and reduced hypoglycaemia awareness in elderly people who take mixed insulins (Ishikawa et al, 2017), but it would appear that this has yet to provoke widespread alteration in insulin regimens or use of innovative technologies to support this vulnerable group.
All community nurses monitor capillary glucose levels at the time of the delivery of insulin injections. In all participants in this case series, blood glucose at this time was below the level considered optimal for frail elderly people, noting recommend therapeutic targets and de-escalation thresholds (Strain et al, 2018). However, at the time of the visit by the community nurse and the administration of the insulin, they were not showing hypoglycaemia. We believe this innovative use of flash monitoring technology adds to published data on the increased frequency of hypoglycaemia with twice-daily mixed insulins in frail elderly patients.
The stopping of insulin within this cohort can be challenging and raised safety concerns regarding the individuals’ own endogenous insulin production. For the two participants who had their insulin stopped, there was an increase in visits by the DSN, who visited the day that the insulin was stopped and within 24 hours afterwards. Ketone meters were provided and a plan put in place to ensure safety.
Summary
The management of this cohort of patients using flash glucose monitoring technology has led to the following:
- An improved understanding of the challenges of consistency associated with administration of insulin by external healthcare professionals in a home environment.
- A safe reduction or cessation of daily insulin doses.
- A reduction in community nursing visits. For the individuals discussed here, there was a reduction of 1460 nurse visits over 1 year. With an estimated cost per visit of £40, this represents a reduction of £58 400 per year just in visits.
- We would expect this approach, in due course, to lead to more rational prescribing of insulin, safe de-escalation of treatment and a reduction in falls and hospital admissions for a frail, vulnerable cohort of people who often live alone.







Study provides new clues to why this condition is more aggressive in young children.
14 Nov 2025