Historically, access to advanced technologies for people with diabetes in the UK has varied according to locality and the local services available (NHS Digital, 2023a). In recent years, however, the NHS has made large strides in this area, particularly for people with type 1 diabetes (Kar, 2024; NHS England, 2024a). This has aligned with developments in continuous blood glucose monitoring (CGM) technologies, their ability to link with insulin pump therapies and the subsequent evolution of hybrid closed-loop (HCL) systems. Such systems use algorithms powered by artificial intelligence (AI) to inform insulin delivery in response to the CGM data (DSN Forum UK, 2024). There is good evidence that HCL therapy can reduce glycaemic variance, improve HbA1c, quality of life and time in range (TIR), and reduce episodes of hypoglycaemia (Boughton et al, 2022; Crabtree et al, 2023; Ng et al, 2023).
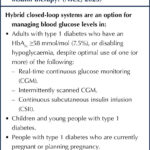
Conventional insulin pump therapy demanded a high level of self-management, and users needed regular reviews and support from a trained specialist team (NICE, 2008). While NICE (2023) guidance also recommends that HCL systems should only be used with the support of a trained multidisciplinary team, the criteria for those who could and should be able to access these therapies has broadened (Box 1). Access remains uneven across age, ethnicity and level of deprivation, suggesting the need for training and awareness (NHS Digital 2023a; 2023b). However, as access to these technologies grows, healthcare professionals in all areas of care will encounter people using HCL systems (Griffin et al, 2023; NHS England, 2024a).
Consequently, the 5-year rollout strategy from NHS England (2024a) recognises the need to train and build specialist competencies within the clinical workforce. A decision-support tool is available to help people with type 1 diabetes decide between different diabetes technologies, with guidance from their diabetes team (NHS England, 2024b).
This article provides essential information for non-specialist staff to support individuals using insulin pump therapy, and in the identification of people who may benefit by from it. It covers how insulin pumps work, some advantages and possible concerns in their use, early identification of emergency situations and signposting to appropriate services. A glossary of terms is provided at the end.
What is an insulin pump?
An insulin pump is a wearable and programmable device that delivers small amounts of rapid-acting insulin at regular intervals throughout a 24-hour period to help manage glucose levels. When linked to a CGM device, it forms an HCL system. This kind of system uses data from the sensor to adjust the basal (or background insulin delivery rate automatically). To do this, the individual’s correction factor (or insulin sensitivity factor [ISF]), blood glucose target range and insulin action time (IAT) must be calculated and entered in the insulin pump’s settings.
The user can also programme the system to deliver bolus (or mealtime) insulin to cover carbohydrates from snacks or meals, or to correct high blood glucose (Breakthrough T1D, 2024a). HCL systems still require the user to announce when they are eating and if activities or health status (Griffin et al, 2023). Although the systems may look different, and use slightly different AI systems and compatible sensor therapy (DSN Forum UK, 2024), they all have similar functions and consist of several components:
- A mechanical pump powered by a disposable or rechargeable battery. It operates like a piston, pushing insulin out of the reservoir according to the pre-programmed settings (basal programme), glucose measurements transferred from the sensor or on operator’s instruction (bolus).
- Reservoir (small container or syringe that holds the rapid-acting insulin within the pump).
- Cannula (small needle or plastic device) that is inserted subcutaneously.
- Tubing (even if hidden) that connects the reservoir to the cannula.
How does it work?
Basal
The basal insulin infusion rate, or basal rate (BR), is adjusted according to the individual user’s requirements at different times of the day. Recent developments in HCL systems allow automation of insulin delivery to maintain blood glucose levels within pre-defined targets throughout the day and night.
Some systems (especially if the HCL system is turned off) allow for more than one basal rate programme to be saved. This can be useful in situations where there may be large differences in activity levels or in insulin requirements (e.g. during illness or when commencing or ceasing certain medications, like steroids). The user can switch easily between the settings according to their activities and glycaemic trends (Diabetes Technology Network UK [DTN-UK], 2018a; 2023).
Bolus
Bolus doses can be delivered by the insulin pump in several ways. Smart algorithms assist in insulin delivery calculations based on the user’s insulin-to-carbohydrate ratio, ISF and target blood glucose levels. This bolus function allows the system or individual to accurately calculate doses and to reduce the risk of insulin stacking (i.e. bolus doses given too close together), as it will also account for insulin still active in their system (i.e. the insulin on board).
Note that these settings may vary through the day. Bolus doses of insulin may be delivered automatically or manually if blood glucose levels are above target, or delivered by the user to cover meals. They can be delivered via the pump as:
- An immediate or correction bolus. This delivers the suggested amount of insulin instantaneously.
- An extended bolus. This delivers the suggested amount of insulin but prolongs the delivery time. It is useful for foods with a low glycaemic (GI) index or those high in fat or protein.
- A combination bolus. This is a mixture of an immediate and extended bolus. It enables the fast-acting carbohydrates to be managed by the immediate part of the bolus and the longer-acting/lower-GI carbohydrates to be managed by the extended part of the bolus.
Note that in some HCL systems the extended and combination bolus function has been removed, as the system will automate the insulin delivery according to sensor feedback once carbohydrate intake is announced (DSN Forum UK, 2024).
Blood glucose variance
There have been a number of developments in diabetes technology. Historical systems used standalone CGM or used CGM alongside insulin pumps. When CGM devices were initially linked to pumps it resulted in the ability to alert the user to low blood glucose and to suspend insulin delivery (the low glucose suspend [LGS] function). Further developments then made it possible to predict low blood glucose levels and suspend insulin delivery before hypoglycaemia occurred (predictive LGS).
Now, HCL systems can increase or decrease delivery according to current glucose levels. Evidence shows that these developments lead to improvements in key indicators of glucose control and well-being.
Hypoglycaemia
The causes of hypoglycaemia are often multifactorial. However, by reviewing the data downloaded from the insulin pump device, the causes of hypoglycaemic events may be identified. It may be attributed to excess insulin administration owing to an overestimation of bolus doses, multiple bolus doses given in quick succession (insulin stacking), a mismatch between bolus insulin administration and food consumption, incorrect insulin pump device settings or exercise (Griffin et al, 2023).
Assuming that the pump settings are correct and the hypoglycaemic event is caused by one of the other reasons listed above, the person would be advised to follow the advice in Table 1 to aid correction of glucose levels. There is generally no requirement to eat longer-acting carbohydrates once the blood glucose level has been corrected. When using an HCL system, it will adjust insulin delivery according to the sensor readings (DTN-UK, 2023). So, if glucose was low, or expected to become low, the system will have already reduced or ceased insulin delivery. This, in turn, reduces the need for additional carbohydrate loading.
If the user is struggling with persistent episodes of hypoglycaemia, they should be advised to contact their specialist team for review as soon as possible.
Hyperglycaemia
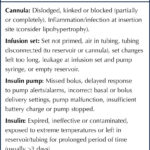
One of the most common precipitating causes of hyperglycaemia with insulin pump therapy relates to cannula failure due to it being displaced or incorrectly inserted (Flores et al, 2020). If not detected promptly, it can lead to a state of insulin deficiency and significantly increase the risk of developing diabetic ketoacidosis (DKA) within a matter of hours (DTN-UK, 2018a; 2023; NHS, 2024). Individuals using insulin pump therapy should be encouraged to explore the reasons for high glucose levels as soon as they are detected. Box 2 highlights some causes of hyperglycaemia and areas that should be explored.

How to identify emergency situations
Illness
It is imperative that insulin pump users are fully aware of sick-day rules and have access to all the equipment discussed in the previous section. They should be advised to:
- Check for ketones if feeling unwell or have unexplainable elevated blood glucose levels >15 mmol/L (e.g. if not related to excess food intake; Griffin et al, 2023).
- If there are no cannula/infusion set issues and no ketones present, correct blood glucose level using the insulin pump, and monitor blood glucose and ketones in 2 hours.
- If ketones are present, administer 10%–20% of their total daily dose (TDD) of insulin (see Glossary, page 6) as a bolus (with a pen device or syringe) every 2 hours, ensuring that insulin is added for any oral intake (using their usual insulin-to-carbohydrate ratio).
Change the cannula and infusion set and, if in open-loop mode, increase the basal rate by 30%–50%. If in closed-loop mode, additional corrections may be needed to manage glucose levels. - Continue to test glucose and ketone levels every 2 hours.
- Continue to correct glucose levels every 2 hours (either using pen device or insulin pump bolus function, as above).
- If using the insulin pump in open-loop mode, actively use a temporary basal rate (TBR).
- Drink plenty of water.
(DAPHNE, 2020; DTN-UK, 2018a; 2018b; 2023)
Remember, the pump does not know when the user is unwell. Therefore, the user will need to manage elevated blood glucose levels proactively. If unable to self-manage this (particularly if associated with elevated ketone levels and/or symptoms of DKA), they must seek specialist advice urgently or present at an accident and emergency department.
Admission to hospital
Over 90% of inpatients with diabetes are admitted for non-diabetes-related issues. Of patients with type 1 diabetes, an increasing proportion are expected to be insulin pump users. They are generally admitted to clinical areas that best fit the cause of admission. Despite a greater focus on training, it is likely that most non-specialists will have minimal expertise in the management of insulin pump therapy. Consequently, if a pump user cannot self-manage their therapy, most non-specialist teams are advised to discontinue it and switch to therapies they are trained to manage (i.e. variable rate insulin infusions or subcutaneous injections of insulin; JBDS, 2024).
There are situations where insulin pump therapy may not be suitable. During MRI scanning, the magnetic fields may cause the pump and sensor to become detached suddenly. Also, induction heat caused by the magnetic field may damage the insulin pump. In such instances, both the insulin pump and sensor should be removed (for a maximum of 60 minutes) and stored safely. Currently, similar guidance exists for CT scanning, although there are considerations for use of lead screening equipment as long as these devices are situated away from affected site (JBDS, 2024). If the insulin pump therapy is expected to be interrupted for a prolonged period (i.e. more than one missed meal), the team should switch to the therapies mentioned above (DTN-UK, 2018b; Centre for Perioperative Care, 2023; JBDS, 2024).
It is important to involve the specialist diabetes teams with any care decisions made for these individuals as soon as possible. In a planned admission, if the specialist team is informed in advance, a treatment plan can be devised with the pump user and relevant healthcare professionals that may enable the individual with diabetes to manage their own therapy.
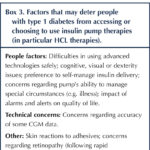
Considerations for initiating insulin pump therapy
To gain optimal outcomes with insulin pump therapy and demonstrate an appropriate use of NHS resources, individuals are assessed for insulin pump and HCL therapies using the latest guidance (NICE, 2023; see Box 1). Historically, insulin pump therapy demanded a high level of self-management, training and education, with regular review and support from a diabetes specialist team. Referrals to pump services may have been impacted by a lack of locally available services and limited understanding of insulin pump therapy, its benefits and complexities (Kar, 2024; NHS England, 2024b). Despite concerns remaining about insulin pump therapy among some people with type 1 diabetes (Box 3), the rapid developments made in device interfaces and usability, and the resulting improvements in outcomes, will significantly increase the number of people who will benefit from these therapies.
The updated guidance suggests that addition considerations should be made for those who, despite support, are unable to manage glycaemic excursions related to the dawn phenomenon or exercise, those with high levels of diabetes distress and those with impaired hypoglycaemic awareness. Specialist teams may also consider the use of insulin pump therapy for people from additional sub-groups of service users, if there is clinical need under NICE guidance NG3 and NG17 (NICE, 2020; 2022) and best practice guidance (Griffin et al, 2023). This includes those who have additional learning needs (who can be supported within some systems with infographics and estimated meal size options).
Travel
Travelling with any advanced diabetes technologies should not be a limiting factor, but does require some extra considerations (Trend Diabetes, 2023; Breakthrough T1D, 2024b; Diabetes UK, 2024b). Pump users should:
- Take 2–3 times the quantity of medical supplies they would usually need (e.g. in case of cannula or sensor failure or emergency). Check in advance if their pump manufacturer has a holiday loan service in case of a breakdown.
- Carry all supplies in their hand luggage, as any loss of luggage could cause significant risk. Remember, insulin put into the hold can freeze, rendering it useless. Obtaining replacement insulin and consumables can take time and be costly.
- Carry an insulin pump-specific letter from their doctor or specialist team. Consider visiting customer services at the airport to access a hidden disabilities lanyard. This will inform security staff of the requirement for insulin pump therapy, provide instructions regarding care and management of equipment, and the need to carry sharps, medicines and emergency treatments. Most insulin pump manufacturers also have letter templates available (many will provide them in specific languages).
- Avoid X-rays/magnetic fields at airport security, as these may damage the integrity of the pump and/or sensor.
- Replace the cannula, tubing and reservoir every 2 days whilst visiting hot climates, as the insulin may deteriorate more rapidly. Problems with cannula displacement may be experienced owing to adhesive issues relating to perspiration.
- Store their insulin supplies in a fridge.
- Use a “temporary basal rate” (TBR) or temporary targets according to their activities and glucose response. Remember that insulin absorption rates are altered in hot/cold climates.
- Adjust the time zones within their pump settings. (Wait until arrival at destination before changing the insulin pump to local time.)
- Switch the pump to airplane mode during take-off and landing. Some manufacturers suggest disconnecting the tubing from the cannula during take-off and landing.
- Arrange travel insurance. Ensure this covers all medications, medical devices and medical assistance.
- Carry medical alert identification. In an emergency, this allows others to identify their needs and seek the right medical attention promptly.
- Take long-acting and rapid-acting insulin pens in their emergency pack in case of pump failure. Take a copy of their insulin pump settings and familiarise themselves with conversion to injection calculations/management, in case of emergency.
Indications for pump discontinuation
Until the introduction of the best practice guidance (DTN-UK, 2018a), there was no clear guidance for clinicians regarding the removal of insulin pump therapy. This led to widespread variance in decisions made by specialist teams. Subsequent guidance (DTN-UK, 2018b; Griffin et al, 2023; JBDS, 2024) recommends that the decision to discontinue insulin pump therapy should be made after discussion with the individual and the whole specialist team. These discussions usually only proceed to discontinuation (either temporarily or permanently) if: there is a concern that insulin pump therapy is not safe; at the pump user’s request; there are recurrent admissions with ketosis or DKA (with no other viable options); and/or there is cognitive impairment. In any of these scenarios, the insulin pump user must be supported by the specialist team with education and psychological support, with the aim of reinitiating insulin pump therapy as soon as possible and if appropriate.
Conclusion
The population of insulin pump users is expected to grow the UK. Despite guidance specifying that users require specialist teams to provide ongoing care and support, there is an increasing and pressing need for non-specialists to possess some basic knowledge to identify emergencies and signpost individuals to appropriate services. This will become more apparent as more people present to non-specialist areas with difficulties. Additionally, with the introduction of the decision-support tool (NHS England, 2024b) and wider training on advanced technologies, many people who may benefit from these therapies will be identified in community and GP settings. This article will assist in the identification and prompt referral of these individuals to specialist teams for further assessment.
To achieve the best possible insulin pump therapy outcomes, users will need a clear understanding of what it is, how it works and how it may aid them to achieve their therapeutic goals.
These devices have proven benefits in reduction of glycaemic variance, improved HbA1c, quality of life and time in range, and fewer episodes of hypoglycaemia. As a result, they have been approved as being clinically cost effective in the groups of individuals for whom they are recommended.
Glossary of terms
Basal insulin: The continuous “background” insulin delivered over 24 hours to maintain blood glucose levels when the user is not eating. While “traditional” multiple daily injection (MDI) therapy uses a long-acting insulin for this purpose, insulin pump therapy uses only rapid-acting insulin.
Basal insulin rate (BR): The rate at which the basal insulin is delivered.
Bolus insulin: A dose of rapid-acting insulin delivered to manage the rise in blood glucose levels that occurs after meals or to correct high blood glucose levels.
Dawn phenomenon: The natural early morning rise in blood glucose that relates to increased levels of stress and growth hormone secretion.
Glycaemic index (GI): Indicator of how rapidly a food source may be digested and speed of impact on glucose levels. Low-GI foods (<50) cause a slower, more gradual rise in glucose levels, while high-GI foods (>70) lead to a faster, higher spike.
Insulin action time (IAT): The total length of time that an insulin dose continues to work in the body.
Insulin correction factor: Also known as the insulin sensitivity factor (ISF), it is how much 1 unit of rapid-acting insulin may lower an individual’s blood glucose level.
Insulin-to-carbohydrate ratio (ICR): How many units of rapid-acting insulin a person needs for a specific amount of carbohydrate to keep their glucose levels stable. For example, an ICR of 1:10 means that 1 unit of insulin is needed for every 10 g of carbohydrate eaten.
Insulin stacking: The accumulation of insulin within the system. Often caused by multiple injections of subcutaneous insulin given before the previous dose has cleared from the system.
Insulin on board (IOB): The amount of insulin that is active in the body.
Lipohypertrophy: A common complication associated with regular injections of insulin. This may cause lumps of fatty tissue to form under the skin. In turn, this can impact the absorption of insulin and result in inconsistency in insulin release.
Open-loop mode: When the insulin pump and sensor data are not directly communicating to automate insulin delivery. Pumps used in manual mode require the user to manually input information to deliver a bolus or suspend/increase basal insulin delivery.
Target range: The ideal upper and lower glucose levels set and agreed with an individual (usually based on international consensus guidance). Time in range (TIR) is the percentage of time that the level is within the target range.
Temporary basal rate (TBR): An insulin pump feature that allows for a short-term adjustment of basal insulin delivery (TBR). This may be reduced in activity (to reduce risk of hypoglycaemia) or increased in illness (to reduce risk of hyperglycaemia).
Temporary target: An adjusted glucose target level to allow a reduction of insulin delivery to reduce the risk of hyperglycaemia.
Total daily dose (TDD): The sum of all insulin (basal and bolus) taken over a 24-hour period.
Acknowledgment
The author wishes to express her sincere appreciation of Professor Pratik Choudhary for supporting her training and ongoing clinical practice in this specialist area.





In her final editorial, Su Down reflects on her career and the remarkable progress in diabetes care she has seen.
11 Dec 2025