What and why
● Gestational diabetes (GDM) affects at least 5% of pregnancies in the UK.1
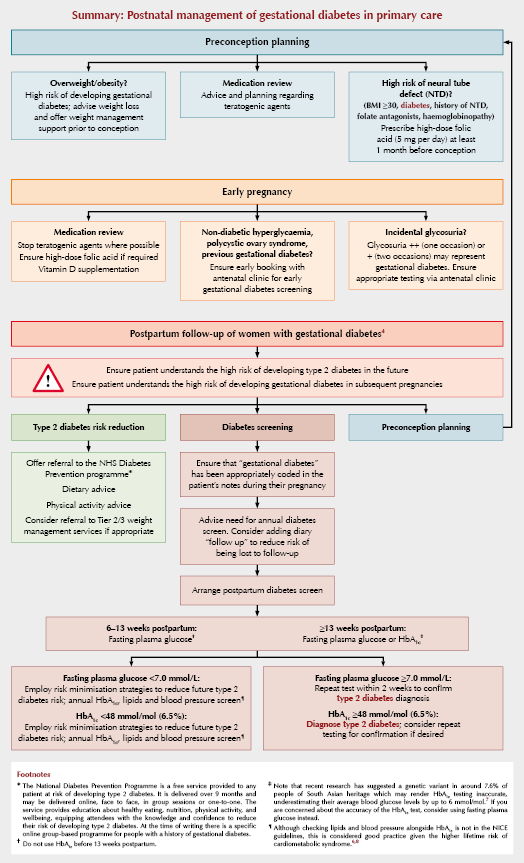
● It is often asymptomatic; therefore, pregnant women at high risk of developing GDM should be screened using an oral glucose tolerance test at 24–28 weeks’ gestation. Those with previous GDM, non-diabetic hyperglycaemia or polycystic ovary syndrome should be advised to seek early antenatal advice for consideration of early GDM screening.
● 50% of women with GDM go on to develop type 2 diabetes within 5 years;1 thus, annual follow-up, counselling and treatment in primary care are essential.
● All women with a history of GDM should be offered referral to the NHS Diabetes Prevention Programme.
What is gestational diabetes?
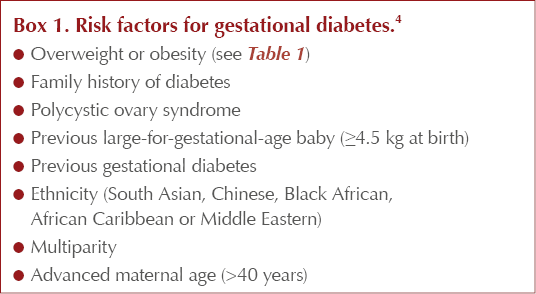
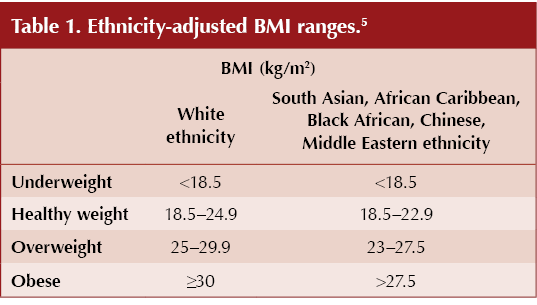
GDM is diabetes which occurs during pregnancy due to a dysfunctional adaptation to the increasing insulin resistance of pregnancy. Risk factors are listed in Box 1. Additionally, women of South Asian, African Caribbean, Black African, Chinese and Middle Eastern heritage are at a higher risk of developing GDM; therefore, lower BMI ranges are applied to mitigate the cumulative risk of overweight and obesity in these cohorts (Table 1).
GDM is associated with complications including emergency caesarean sections, shoulder dystocia, instrumental delivery, pre-eclampsia, stillbirth and increased risk of childhood obesity and diabetes in offspring.
Why do we need to follow up GDM?
Women with GDM have an increased lifetime risk of cardiometabolic syndrome, with up to 50% developing type 2 diabetes within 5 years.1 Type 2 diabetes is associated with cardiovascular disease, stroke, nephropathy, neuropathy, retinopathy and cancer; over 6% of the UK health budget was spent on diabetes in 2021/2022, with the majority spent on treating preventable conditions.2 With approximately 1.2 million people living with undiagnosed type 2 diabetes in the UK, it is imperative that those at high risk are followed up appropriately.3
Postpartum follow-up
Type 2 diabetes screening
NICE NG3 guidance recommends fasting plasma glucose testing between weeks 6–13 following delivery, or either fasting plasma glucose or HbA1c after 13 weeks (Table 2).4 HbA1c should not be used before 13 weeks following delivery, as this will provide an inaccurate result.
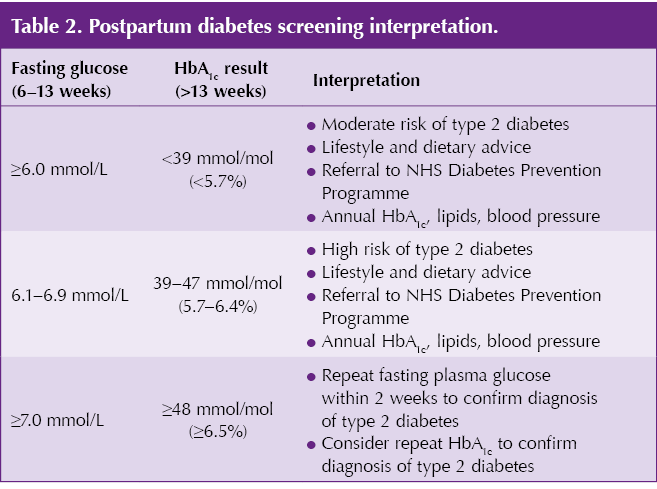
South Asian women are nearly twice as likely as White women to develop type 2 diabetes within 5 years.6 This is important to recognise, as a genetic variant in around 7.6% of people of South Asian heritage may render HbA1c results inaccurate, underestimating their average blood glucose levels by up to 6 mmol/mol and delaying their diagnosis of type 2 diabetes.7 Where there is concern about the accuracy of the HbA1c test, consider using fasting plasma glucose instead.
Cardiovascular risk assessment
Increasing evidence demonstrates an association between GDM and lifetime risk of adverse cardiovascular outcomes and dyslipidaemia, with Black women nearly three times more likely than White women to have high blood pressure following a GDM diagnosis.6,8
Although lipid and blood pressure screening are not currently part of national guidance for the postpartum annual follow-up of GDM, the author argues that they should be considered, alongside annual HbA1c, in light of this evidence.
Type 2 diabetes prevention
All women with a history of GDM should be offered referral (or can self-refer) to the NHS Diabetes Prevention Programme.1 This is a free, 9-month course providing proven, structured diabetes risk reduction education to anyone with a high risk of developing type 2 diabetes. Referral to Tier 2 and Tier 3 weight management programmes should also be considered where appropriate.
Mental health
Women with a history of GDM may have found their pregnancy and labour difficult or traumatic, and research has found an increased risk of developing postpartum depression.9 It is important to recognise this and ask about it directly during the postpartum appointment to ensure appropriate support and follow-up.
Further considerations
❑ Are you confident that all women with a history of GDM have an appropriate corresponding code in their notes?
❑ Are you confident that all of your patients with a history of GDM have had their annual diabetes screen?
- An Ardens search template is available which highlights patients with a historical code of “gestational diabetes” who have not had their annual blood test.
❑ Children born to mothers with GDM are at higher risk of developing childhood obesity and diabetes. It is worth keeping this in mind and ensuring adequate weight management and healthy lifestyle counselling for families.
Useful resources for women with GDM
● Diabetes UK Gestational diabetes:
https://www.diabetes.org.uk/diabetes-the-basics/gestational-diabetes
● NHS Diabetes Prevention Programme self-referral link:
https://preventing-diabetes.co.uk/referral/history-of-gdm/
● Trend Diabetes At Risk of Diabetes:
https://trenddiabetes.online/portfolio/at-risk-of-diabetes/
● British Heart Foundation recipes:
https://www.bhf.org.uk/informationsupport/heart-matters-magazine/nutrition
● Patient.Info dietary advice:
https://patient.info/diabetes/type-2-diabetes/type-2-diabetes-diet
● Free NHS Weight Loss Plan mobile app:
https://www.nhs.uk/better-health/lose-weight/
● Tommy’s Planning a pregnancy after gestational diabetes: https://www.tommys.org/pregnancy-information/im-pregnant/planning-pregnancy-if-youve-had-gestational-diabetes
● Birth Trauma Association:
https://www.birthtraumaassociation.org
Acknowledgement
The author thanks Nicola Milne (DiaST Lead, Brooklands and Northenden PCN) for her review prior to publication.
Summary: Postnatal management of gestational diabetes in primary care





Jane Diggle discusses emotional health and diabetes distress, and offers some tips for discussing this in our consultations.
11 Nov 2025