The term “diabetes distress” has been defined by the American Diabetes Association (ADA; 2021) as:
“…significant negative psychological reactions related to emotional burdens and worries specific to an individual’s experience in having to manage a severe, complicated, and demanding chronic disease such as diabetes.”
Diabetes distress has been found to be more prevalent and persistent than major depressive disorder, and it can have a huge impact on diabetes management (Rariden, 2019). Diabetes burnout is a state of physical or emotional exhaustion caused by the continuous distress of diabetes, as well as efforts to self-manage it. People with diabetes (PWD) may feel that, despite their best efforts, their blood glucose levels are unpredictable and disappointing; this often leads to feeling helpless and disengaged from diabetes self-management (Polonsky, 1999). People with diabetes burnout can feel disheartened with the continual effort required to manage diabetes. This state of mind can be temporary or impact continuously. Healthcare professionals (HCPs) can describe people with diabetes burnout as “difficult”, “non-compliant”, or “unmotivated”, while they are actually struggling with following the long list of tasks that are necessary to manage diabetes (Abdoli et al, 2020).
People with diabetes burnout can disengage from nutrition tasks, such as carbohydrate counting or eating healthily, among other diabetes-related tasks. They can present with eating disorders or risk-taking behaviours and, furthermore, it might be hard to engage them in attending clinics and discussing their diabetes management (Polonsky, 1999).
The best way to avoid diabetes burnout is to regularly screen for diabetes-specific distress, so that advice and support can be offered by the diabetes team in a timely manner.
Nutrition burnout
Unlike “diabetes burnout”, there is not a specific term that describes “nutrition burnout”. Yet this is very important for dietitians to consider, as often PWD can be struggling solely with the tasks involved in nutrition therapy, rather than their diabetes as a whole.
One of the key approaches of nutritional therapy when living with type 1 diabetes (T1D) and using intensive insulin therapy is to match the insulin dose to carbohydrate intake, in line with individualised insulin-to-carbohydrate ratios (level 3 carbohydrate counting [CC]). It is recommended that this is taught from diagnosis to all children and young people (CYP) with diabetes (NICE, 2016).
Carbohydrate counting
CC aims to improve glycaemic control and gives flexibility of food choices (Tascini et al, 2018). However, CC can be difficult for families, and the education should be adapted to their culture, preferences, capacities and understanding.
In a study by Fortin et al (2017), which involved adults with T1D, there was a relationship between the level of confidence in doing CC with the education level. In the same study, participants who had depression found that CC was harder to perform in their daily lives. According to the study, the factors that made CC difficult were the impression that glucose levels were fluctuating even with CC and that CC complicates the management of diabetes (Fortin et al, 2017).
Common barriers for CYP that can impact adherence to CC include peer influences, social context and depression (Borus and Laffel, 2010).
Intervention strategies should address the individual’s goals and expectations of using CC as part of intensive insulin therapy, emphasise problem solving to manage the challenges of dining out and changes in daily routines, and provide practical and applicable CC resources (Leung et al, 2014).
CC is not the only task that PWD should consider in their daily routines. The fat and protein content in meals has also shown to have an impact in insulin dosing decisions (Figure 1).

Role of healthcare professionals in avoiding nutrition burnout
PWD should be routinely assessed for diabetes distress, especially when complications arise (ADA, 2019). Routine monitoring and discussing diabetes burnout with individuals with T1D have also been suggested to improve psychosocial wellbeing and diabetes outcomes (Abdoli et al, 2021).
One such method could be dietitians teaming up with psychologists to explore if different aspects of the distress are related to nutrition tasks. If this is done in a timely manner, it could prevent burnout in CYP with T1D. Parental anxiety can also have a direct and negative effect on diabetes management and health outcomes (Sundberg et al, 2017). This is why it may be important to consider assessing parental diabetes distress too.
For example, if using the Problem Areas In Diabetes (PAID) Scale for Children (PAID-C; Evans et al, 2019) or PAID for Teenagers PAID-T; Shapiro et al, 2018) and parents’ version questionnaires, some of the statements can be related to nutrition tasks. These questionnaires have been adapted from the PAID scale by Welch et al (1996) for use with adolescents, children and their parents.
The PAID-T and parent-of-teenager version (P-PAID-T) are valid and reliable measures for use in adolescents and their parents. The PAID-T has a three-factor structure of diabetes distress, including the day-to-day burden of managing diabetes tasks (regimen-specific distress) and the perception that one’s family or friends are unsupportive with regard to diabetes management (family and friends distress).
The PAID-C and the parent version (P-PAID-C) show unique factor structures given the developmental differences between the two age groups (Evans et al, 2019). If the child, adolescent or parent answers that some of those related statements are a problem, the HCP can find ways to help. If statements that can be related to nutrition tasks are a problem for the PWD or parents, the HCP can discuss links between emotions and behaviour. Techniques including exploration, identifying feelings, reflection, normalisation and double reflection are suggested. Assessing for distorted beliefs or unrealistic goals and proposing a focused plan which is targeted, attainable, short-duration and with minor modifications is recommended (Rariden, 2019). Table 1 gives suggestions of identifying problem areas in diabetes related to nutrition tasks and suggestions of support to families.

Language matters when speaking about nutrition
HCPs should lead conversations with PWD to identify the connection between their emotions and the hurdles of diabetes management. In starting such conversations, an HCP should consider their approach and use of language, as PWD can find reassurance in feeling they are supported.
Good use of language – including verbal, written and non-verbal – can lower anxiety, build confidence, educate and help to improve self-care (NHS England, 2018). Often, when messages received from a number of different sources, including the media, people around them and HCPs, are perceived negatively, this can lead to feelings of shame, guilt and resentment in the PWD.
PWD often feel criticised or judged by others, including their HCP, regarding their food choices and eating habits (Doherty et al, 2020), so it is important that they feel encouraged to express their concerns in a safe, non-judgemental environment (Odiase et al, 2020).
The PDPEAS (Paediatric Diabetes: Positive Eating, Activity, Self) working group, comprising psychologists and dietitians, has created some helpful resources for CYP with diabetes and their carers (Children and Young People’s North West Diabetes Network, 2021). The working group suggests promoting principles of connected eating to change current nutritional messages delivered through diabetes education. This way CYP living with T1D are encouraged to develop or maintain a healthier relationship with food and their bodies.
Health literacy and language barriers when speaking about nutrition
Health literacy is a person’s ability to understand and apply health-related information and their ability to navigate the health system (World Health Organization, 2013).
After a diabetes appointment, the PWD and/or their carers need to remember everything that took place and was said during the consultation. They then need to apply what they have learnt when they go back home. This could be challenging for a person who has not clearly understood the message that their HCP has tried to convey to them, and this might impact on their self-care and health outcomes (Odiase et al, 2020).
The HCP should analyse if the information was understood, find different ways of explaining nutritional therapy and make adjustments to accommodate individual differences in learning style. CC might include a lot of calculations and also the understanding of the relationship between insulin and foods.
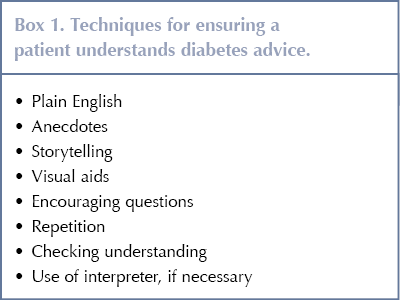
Some techniques and suggestions are highlighted in Box 1 to help PWD feel confident in completing diabetes-related tasks (Misra-Hebert and Isaacson, 2012). Building confidence and understanding can decrease the chances of the person feeling distressed by the tasks.
Dealing with nutrition-related tasks after diagnosis
In the local diabetes clinic, data were collected from 18 newly diagnosed children with diabetes (ages 8–18 years) and their families. They were asked about how they were coping with nutrition tasks after being diagnosed with T1D:
- 40% of the respondents said that the diabetes management task hardest to apply was CC, followed by glucose monitoring and insulin application.
- 22% of the families reported having felt tired or exhausted of making decisions around mealtimes.
- 28% reported having felt that they “can’t be bothered” to use CC.
- 33% of the families have felt worried or anxious about eating outside home (restaurants, school and activities).
- 33% of families have felt angry or upset when CC has not resulted in high or low blood glucose levels.
The families were also asked about the support from the diabetes team in adapting the healthy eating recommendations to their traditions and lifestyle:
- 50% of the families felt “completely supported”.
- All families responded they felt supported to some extent.
The families also shared the different ways they make nutrition-related tasks, such as CC, adapt to their individual lifestyle. Some of the answers are shared below:
“Having a booklet in my lunch box that everyone can see and record my carb count in, at school and home.”
“Using carb-counting apps.”
“Eating similar food portions and learning to memorise the carbohydrate content.”
“Calculate carbohydrates in favourite recipes and dishes using apps.”
“Do a list of favourite takeout menus and the carb content and keep it on the phone.”
For future research, it would be helpful to consider the level of involvement and support of caregivers in those CYP with nutrition burnout. These families would most likely benefit from more contact with the diabetes team.
Eating disorders in CYP with type 1 diabetes
CYP with diabetes appear to have a greater incidence of depression, anxiety, psychological distress and eating disorders (ED) compared to their peers without diabetes (Delamater et al, 2018). There is also an increased risk of ED in CYP with elevated levels of diabetes distress, high HbA1c and body dissatisfaction (Araia et al, 2020).
Diabetes itself could be a risk factor for developing ED, due to the required behaviours related to diet, including the emphasis on dietary management (type, quantity and quality of foods eaten, as well as timing of food intake); possible dietary restraints (restriction of food intake and adoption of dietary rules); focus on weight at diabetes clinic appointments and weight changes before and after diagnosis; the effect of diabetes on self-image and family interaction and other nutrition-related issues (Coleman and Caswell, 2020). By screening for diabetes distress and burnout in nutrition-related tasks (Table 1), HCPs can also detect any signs of eating disorders.
Role of carers in avoiding “nutrition burnout”
Parents and carers of pre-school children can find nutrition-related tasks very challenging due to “normal” food-related issues, such as seeking independence, transient food preferences, variable appetite, food refusal and behavioural resistance (Patton et al, 2008).
Children can recognise parental stress and quickly learn to use their diabetes as a way of getting their favourite foods. It is important for parents to ask themselves, “If my child did not have T1D, would I say no to this request?” (Sundberg et al, 2017). HCPs should work together with parents and facilitate helping techniques when the nutrition-related tasks have been causing distress in the family.
A failure to find the balance in responsibility for diabetes care between the parent and the CYP can lead to increased diabetes distress for all family members (Law et al, 2012). Channelling a pathway towards independence in dietary self-management, through better sharing of adolescent–parent responsibilities for diabetes care, with a timely transfer from parent-dominated to adolescent-dominated self-care, is a crucial foundation for good health-related diabetes outcomes.
Sociodemographic family factors, such as single-parent households or higher family density (more young people than adults in the household), lower family income and ethnic minority status, are associated with less optimal parental involvement in diabetes management (including nutrition-related tasks) and greater risk of poor diabetes management (Delamater et al, 2018).
The involvement of the parents and carers, as well as the school, in nutrition-related tasks can positively impact how the CYP with diabetes copes with their daily routines. Knowing that the tasks are not solely on the person’s shoulders and that support can be found in decision making can allow for the person to feel comforted with a rest from continuous health demands, and thus taking a step away from feeling burnt out.
Conclusion
Even though “nutrition burnout” is not an established term, it is important for HCPs to work together with CYP with diabetes and their carers to avoid stress related to nutrition-related tasks. The HCP should evaluate distress and use appropriate language, considering health literacy and language barriers, to give education about nutrition. It would be helpful to create a tool for CYP with T1D and their carers to evaluate nutrition burnout solely, or as a major component of diabetes burnout, and put into practice different ways of avoiding and dealing with it.
Acknowledgements
Children’s and Young People Diabetes Care Module, Birmingham City University and the collaborating clinical and academic module team.






NHSEI National Clinical Lead for Diabetes in Children and Young People, Fulya Mehta, outlines the areas of focus for improving paediatric diabetes care.
16 Nov 2022